
Share
Tweet
Share
Share
How America’s prisons are fueling the opioid epidemic
tweet
share
For once, Casey is optimistic about his future. After 16 years of struggling with drug addiction, he no longer feels the need to use. He has a steady job doing hazard tree removal for a Fortune 500 energy company. He’s working on getting specialized training for a license to help him land better-paying jobs. He’s even going to the gym.
But Casey, who asked that I only use his first name for this story, knows this could have turned out very differently. In fact, it had the past few times he was released from prison. Before, he had relapsed as quickly as a matter of days — not only exposing himself to the risk of a deadly overdose but leading to a spiral of drug use that hindered just about every aspect of his life and, often, landed him in prison again.
The big difference: This time, he got treatment — real treatment — while he was in prison.
Casey, who’s 36, was one of the beneficiaries of Rhode Island’s relatively new approach to treating opioid addiction in prisons and jails: It now provides the three main medications for opioid addiction to inmates within its facilities, with few strings attached. The three medications — buprenorphine, methadone, and naltrexone — are considered by experts to be the gold standard of care for opioid addiction, with studies showing that they reduce the all-cause mortality rate among opioid addiction patients by half or more and do a far better job of keeping people in treatment than non-medication approaches.
“If I tried doing it on my own, I would have relapsed,” Casey told me. “I hate saying that, because I’m a mentally strong person — you know, I can go through the wringer. But after six or seven or eight years of doing this to myself, all of a sudden when I get clean [without medication], I just don’t feel 100 percent. I’m stuck at 90.” He said that buprenorphine, which he started taking after he was incarcerated in November, keeps him at 100 percent without using other drugs.
Rhode Island’s approach is unusual. In an extensive review of state prison policies, I found that almost no state prison system offers these medications to inmates suffering from opioid use disorder. Only Rhode Island credibly reported providing full access to all three kinds of medication. The great majority of states reported not fully providing any medication at all or allowing only naltrexone, the medication with the least evidence behind its effectiveness.
Related
I looked for a state that’s taken the opioid epidemic seriously. I found Vermont.
In other words, the majority of state prisons don’t offer full access to what experts say is the mainline form of treatment for opioid addiction — and the kind of treatment that has helped Casey get his life back in order.
Before this, Casey had struggled with addiction for 16 years, starting with OxyContin and progressing to heroin and other substances. In that time, he was arrested four times for drug possession, and he was held in prison for a few weeks or months at a time. He would be “clean,” he said, initially during his release — since he was forced to detox in prison — but within days or weeks, he’d be back to using drugs.
With buprenorphine treatment that began with his most recent stint in prison, Casey has managed to avoid relapse since he was released in mid-January. “I don’t feel the cravings like I did before,” he said. “It’s really helped me to stay clean.”
In some ways, Casey is lucky — he survived to this point. Since so few state prisons offer adequate access to treatment, the days and weeks after a person’s release from prison are perhaps the single deadliest time period in the US’s opioid epidemic.
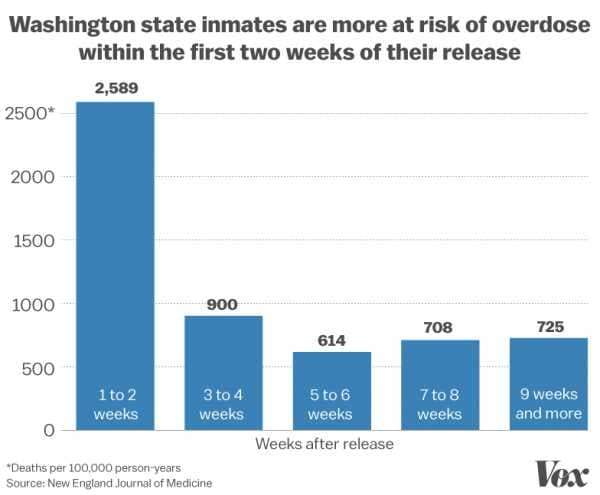
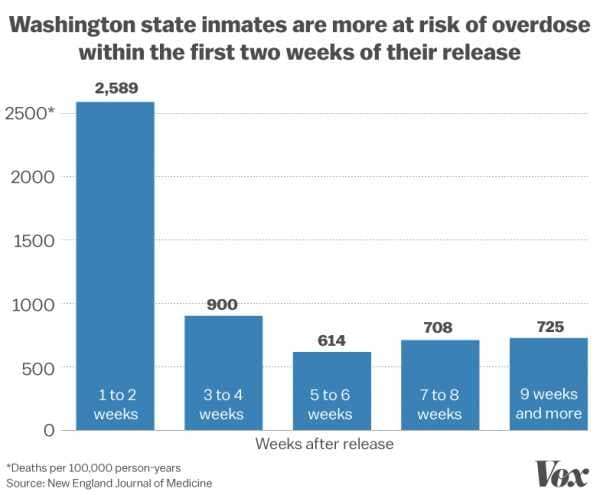
When an inmate addicted to opioids is released from prison, his chances of a fatal overdose are massively elevated: According to a 2007 study published in The New England Journal of Medicine, former inmates’ risk of a fatal drug overdose is 129 times as high as it is for the general population during the two weeks after release. Other studies have backed this up, putting the increased risk of overdose death in the tens of times or above 100 times.
“Globally, there is no more high-risk period and no more high-risk population than those leaving incarceration,” Traci Green, a researcher at Brown University in Rhode Island, said. “It’s during those first two weeks and out to four to six weeks that people are at greatest risk of overdose death.”
Although Rhode Island’s program is still young, a recently released study found that it seems to work as expected — cutting overdose deaths among released inmates by more than half. In Casey’s telling, the program has helped mitigate his risk here as well.
Yet Rhode Island’s approach remains rare, even in the midst of an opioid crisis that was linked to at least two-thirds of 2016’s record 64,000 drug overdose deaths.
“We have a population that’s incredibly vulnerable,” Sarah Wakeman, medical director at the Massachusetts General Hospital Substance Use Disorder Initiative, told me. “It’s really inexcusable that we don’t make this available for people who are at such risk of death.”
Most state prisons don’t fully offer medications for opioid addiction
Over the past two months, I reached out to the 50 agencies behind state prison systems, where around 1.3 million people are locked up. I first asked them if they provided any of the three main medications for opioid addiction — buprenorphine, methadone, and naltrexone. If so, I followed up to see if there were any restrictions attached. If necessary, I also verified what states said with news reports, state laws and regulations, and local experts or activists.
Of the 46 states that sufficiently responded to my initial questions and follow-ups, only Rhode Island reported full access to all three forms of opioid addiction medications. Hawaii said that it allows, at least in theory, buprenorphine and methadone, although the state clarified that it’s felt little need to widely provide the medications since it hasn’t been hit relatively hard by the opioid crisis. Sixteen states offer only naltrexone. The remaining 28 don’t fully offer any medication to prisoners with opioid use disorders. (You can see states’ responses here.)
Generally, states were counted on the map if they offered the medications — with few restrictions — for inmates diagnosed with an opioid use disorder or inmates who were otherwise taking part in treatment.
For buprenorphine and methadone, that means an inmate with an opioid use disorder should be able to reliably obtain either drug while incarcerated. Both medications work similarly: As opioids themselves, they help stave off withdrawal and cravings, which are two major causes of relapse, without producing the same kind of high that heroin does. This lets a patient focus on other aspects of life without being consumed by a constant desire to use drugs.
For naltrexone, an inmate should be able to obtain the medication at least shortly before his release, although some state prison systems also provide it during an inmate’s entire incarceration. Generally, naltrexone is primarily used to block the effects of opioids — potentially for up to 28 days with the once-a-month shot Vivitrol — although it can also reduce cravings.
States were not counted as providing medications on the map if they imposed strict limits on how long an inmate could be on the medications, offered the medications as part of small pilot programs, allowed the medications only for certain groups (such as pregnant women or people who were on medications prior to incarceration), or provided the drugs exclusively for detox or withdrawal management.
In addition to the states, the federal Bureau of Prisons (BOP) — which takes federal and Washington, DC, inmates — told me that it’s only working on a small program to provide naltrexone to inmates in federal facilities: “Specifically, inmates will begin treatment just prior to transferring to a Residential Reentry Center (RRC) and will continue the treatment for several months in the RRC. The program will begin in Boston and to the extent resources are available and the program is found to be effective, the BOP will look to expand the program.”
One caveat: The map shows the states that technically allow certain medications, but whether a drug is truly accessible — meaning someone can actually obtain and fill a prescription in prison — is going to vary from state to state and even prison to prison. So the map, as dismal as it already is, likely overstates the level of access to opioid addiction medications in state prison settings.
The map also doesn’t cover most jails or parole and probation, both of which are sometimes leveraged by authorities to link people to addiction treatment. This is a very large segment of the correctional population — constituting millions of people — but policies in these areas are often guided by individual courts, probation and parole officers, and local officials who run jails, rather than state prison policy.
But the map is in line with other data. About 58 percent of people in state prison meet the definition for drug dependence or misuse, compared to 5 percent of the general population, according to a 2017 report from the Bureau of Justice Statistics. Yet a 2017 study by Johns Hopkins researchers found that less than 5 percent of people who were referred to opioid use disorder treatment through the justice system received methadone or buprenorphine, compared to nearly 41 percent of people referred through other sources.
The results ripple through society — exposing people to a higher risk of death and other addiction-related problems, as well as imposing higher social and financial costs on other systems that have to pick up prisons’ slack.
How state prison policies can kill people with opioid addiction
There are two big ways that state policies blocking off opioid addiction medications cause more overdose deaths.
First, there’s the risk of overdose within prison. Although studies suggest that drug use is actually lower in prison (since it’s simply much harder to obtain drugs), there is still some drug use — which, obviously, carries the risk of overdose and death. But if someone gets treatment for opioid addiction, he’s going to be less likely to use drugs or overdose while incarcerated.
A bigger concern, though, is the risk of overdose once someone is released from prison — a time period when someone’s risk of death is massively increased.
“The minute people leave, they’re facing tremendous stressors,” said Wakeman, who’s worked with previously incarcerated populations. “They cross over this threshold of leaving this very artificial environment, going back to their usual environment, and with the incredible stress and burden of having just experienced incarceration and trying to pick up relationships and dealing with barriers with housing and employment and insurance. Not surprisingly, cravings come back, and people often relapse very quickly.”

Imagine that an inmate is using heroin or already on buprenorphine treatment before he’s incarcerated. Once he’s locked up, he’s forced off the drugs cold turkey. He actually manages to stay drug-free in prison. But then, a few months or years later, he’s released. He’s thrown back into the same environment where he used drugs. He’s perhaps not sure how to reintegrate into society, creating a lot of stress. But he knows how to get in contact with his old drug dealers.
He does just that — and buys heroin (or, increasingly likely, illicit fentanyl). But since he hasn’t used opioids during all his time in prison, his tolerance is much lower. So when he tries the same dose that he used in the past — or even if he tries to be careful — he’s much more likely to overdose and die.
Buprenorphine and methadone make this much less likely because, as opioids, they help maintain some level of tolerance as long as someone is on them. And naltrexone blocks the effects of opioids altogether. In case of relapse, either of these features would help — the maintained tolerance will allow someone to take a higher dose of heroin, fentanyl, or other opioids without overdosing, and the blocking effect can stop someone from getting high or overdosing at all.
And by reducing cravings in the first place, these medications also reduce the chances of relapse overall.
One thing to keep in mind: Overdose deaths are a tragic proxy for general problems with addiction here, but addiction has many more effects. It destroys people’s careers, drives them to crime, breaks up families, and causes secondary health problems like HIV/AIDS and hepatitis C from reused needles, among many other issues. All of these problems are also made much more likely when people can’t get access to adequate treatment.
In Rhode Island, an alternative — and lifesaving — approach
Rhode Island has shown there is a better way. The state committed serious resources to not only provide all opioid addiction medications in theory, but to make sure they’re accessible to all inmates who need them. And, going further, the system tries to ensure ex-inmates are linked to treatment and continue getting medications as needed after they’re released.
In 2015, Rhode Island Gov. Gina Raimondo, a Democrat, established a drug overdose task force, bringing in major stakeholders to study and implement the best policies to reverse the opioid crisis. Among the proposals was dramatically improved access to opioid addiction medications in state prisons. Over 2016 and 2017, Rhode Island finally scaled up its prison program.
“This has really been my vision for the last 20 years,” said Jennifer Clarke, who has been with the state’s Department of Corrections for two decades and has served as medical program director for two years.



The first evaluation of the system, released in February, reported very promising results: The research letter, published in JAMA Psychiatry, found that in the first six months of 2016, 26 people who were recently released from prison died of a drug overdose. In the first six months of 2017, nine individuals died. This was a drop in mortality of more than 60 percent — far higher than the overall state drop in overdose deaths during the same time period of about 12 percent.
The study has some serious limitations. It was a small sample size. It only looked at the early results of Rhode Island’s program. There was also a drop in the supplied amount of naloxone, the opioid overdose antidote, among released inmates — which state officials copped to a temporary shift in recording practices — that could have mitigated the benefits of Rhode Island’s program.
But this is in line with what you would expect from increased access to opioid addiction medications, given that studies show the death rate tends to drop by half or more when patients get access to these drugs.
Rhode Island shows how to do this right
The key to Rhode Island’s success, state officials said, is that it offers all three kinds of opioid addiction medications.
Casey’s experience speaks to this: He tried to get on methadone in the past, but it just didn’t work very well for him, and he would soon be back to using drugs even while he was on methadone. “I’m not trying to knock methadone at all,” Casey said. “It was just different for me.”
This isn’t atypical in health care. It’s often true that what works for one patient won’t for another. That’s why it’s important, experts say, to provide as many options as possible — as Rhode Island has done with its in-prison treatment program. Many people may do well on methadone, others may prefer buprenorphine, and yet some may find the best results with naltrexone or even no medications at all.
“It’s critical to have all three of those components available,” Jody Rich, a researcher in Rhode Island who’s involved with the state’s program, told me.
Yet the great majority of states that make any medication possible only offer naltrexone, typically for use as an inmate nears release — even though the best data suggests that, if anything, naltrexone is worse than the other medications. A 2017 study in The Lancet that compared buprenorphine and naltrexone, for example, found that while both medications have similar levels of effectiveness once people are on them, people were more than four times more likely to initially drop out of using naltrexone treatment than buprenorphine treatment.
There’s a straightforward explanation for why buprenorphine performed so much better on the latter count: While buprenorphine requires only partial withdrawal (usually 12 hours to two days of no opioid use), naltrexone requires full detoxification to use (usually three to 10 days). Withdrawal is grueling and, in fact, a major reason for continued opioid use — so it’s no surprise that people would do anything they can to avoid it, even if it means dropping treatment.



Rhode Island’s data speaks to this. It offers all three forms of medication, and naltrexone is far and away the least popular. According to the recent evaluation, just four inmates in the first six months of 2017 opted for naltrexone. In comparison, 180 took methadone and 119 took buprenorphine.
“The most important factor about this medication is what you are going to take,” Rich said. “And so the best predictor of which medication someone will take is actually the patient’s preference.”
Naltrexone is still much better than nothing, but providing all three medications is what makes Rhode Island’s program unique — and, at least so far, very successful.
Beyond providing all three medications within prison, officials also take steps to ensure inmates can get treatment once they’re released — by following up with them, helping them stay on insurance, and letting them use the same clinic they used in prison if needed. This kind of access is key to the program, Rich said.
But the US struggles here too. According to a 2016 report by the surgeon general, just 10 percent of Americans with a drug use disorder obtain specialty treatment, in large part due to a lack of supply in care. And other data shows that even when drug addiction treatment is available, fewer than half of facilities offer opioid addiction medications as an option. The lack of access to adequate treatment outside of prisons will need to be addressed along with access inside of prisons to fully address the opioid crisis.
Skeptics may argue that Rhode Island is a small state where, as a result, this model is uniquely able to work. But this model could be scaled up; it’s just a matter of building more and bigger clinics to cover wider geographical areas and larger populations — not just in prison but outside too. After all, other places, such as Vermont and France, have managed to scale up medication treatment.
“This is a proof of concept,” Rich explained. “If you can get enough people onto these medications, that will reduce overdose deaths.”
Stigma drives prisons’ resistance to offering medications
Although the Supreme Court has found that prisoners are entitled to proper health care, medical services in prison are far from ideal — as prisons avoid paying too much for even lifesaving interventions to reduce expenses. But my investigation suggests that opioid addiction treatment is in especially bad shape, given that prisons in most states don’t even attempt to look like they offer the standard of care.
One big reason for the dire circumstances is stigma. Looking at the research in this area, the White House’s opioid epidemic commission concluded in 2017 that “negative attitudes regarding [opioid addiction medications] appeared to be related to negative judgments about drug users in general and heroin users in particular.”
There are several layers of stigma here. First, there’s the fact that these are prisoners, which simply makes it much harder for people to empathize with them. Of course, many inmates are in prison because of their drug use; for example, about 39 percent of people in state prison for property offenses said that they committed their crimes to get drugs or obtain money to get drugs. Good treatment, then, could actually reduce crime, benefiting not just the inmates but society as a whole. But understanding all of this requires a willingness to empathize with prisoners — which is just not how the US justice system is currently built.
Then there’s the fact that these people are drug users. For a long time, American society has demonized drug addiction as a moral failure — not the disease that health care groups, including the American Medical Association and American Psychiatric Association, agree it is. This moralization of addiction makes it a lot easier to blame the victim for a drug use disorder, instead of blaming the medical condition itself and focusing on treating it.
Finally, there’s stigma against buprenorphine and methadone. Since both are opioids, their use to treat opioid addiction is often described as “replacing one opioid with another” or “replacing one addiction with another.” This misunderstands how addiction works — the defining problem of addiction is not opioid or drug use, but rather when opioid or drug use leads to bad social and personal health and safety outcomes. After all, plenty of people use drugs, from medications to caffeine to alcohol, with few issues.



An example of this stigmatization comes in one of the exceptions that prison systems carve out for opioid addiction medications: pregnant inmates. In my correspondences with state prison systems, they often told me that they’ll allow pregnant inmates to stay on or even start buprenorphine or methadone to avoid withdrawal — even if the rest of the inmate population is not offered either. The reason: Forced withdrawal during pregnancy could hurt or even kill the baby.
Consider the underlying assumption here: The inmate is to blame for her opioid addiction — even though it’s, by definition, a disease she has little to no control over — so it’s okay if she suffers and even dies. The baby, meanwhile, is obviously innocent, so everything must be done to save it, even if it means using a stigmatized form of addiction treatment.
“It sheds light on the fact that for all the many reasons you hear people give for why medication treatments either aren’t offered or shouldn’t be offered in prison, at the core of the argument is this notion that people are undeserving of compassionate, patient-centered, and effective treatment,” Wakeman said. “We have lifesaving, effective treatment that we wouldn’t withhold from babies … yet we’re not making it available.”
There are other issues as well. Prisons don’t have an incentive to care about this problem, since many of the overdoses that happen as a result occur once an inmate is released — out of the prison’s jurisdiction.
There are also worries about inmates and staff diverting buprenorphine and methadone to illegally sell it to inmates. But Rhode Island said that it cut down on this kind of diversion by better monitoring the administration of these drugs. Better access to treatment could even reduce diversion, since some research shows that many people only resort to illegal means of getting buprenorphine or methadone because they don’t have adequate legal access.
Prisons also have concerns about the cost. Rhode Island’s program, for one, costs $2 million a year. (Although that’s only about 0.02 percent of the state’s operating budget.)
But especially given Rhode Island’s success so far, drug policy and public health experts aren’t persuaded by the explanations and excuses for not providing full opioid addiction treatment in prison.
Prisons “are responsible for [inmates’] health care,” Keith Humphreys, a drug policy expert at Stanford, told me. “If they had high blood pressure, [prisons] wouldn’t be allowed to stop them from getting their blood pressure medication. You’d have to supply that. So if they are addicted to opioids, you should have to supply whatever medication they take for that.”
Otherwise, he added, the justice system is “potentially sentencing people to their death.”
Update: Changed New Jersey’s status on the map to “no data” after hearing conflicting reports on its program in further follow-ups.
Sourse: vox.com






