
There’s a surprisingly big disconnect between how obesity researchers think about the causes of and treatments for obesity and how the American public does.
Researchers think some people have genetic and hormonal traits that make them more susceptible to obesity. They view obesity as a complex, chronic disease, like cancer, with many causes and subtypes. They’re also losing faith in dieting and exercise, neither of which is very helpful for weight loss in the long term.
The public, on the other hand, generally believes obesity is caused by a lack of willpower, and that it can be fixed with gym memberships and trendy diets. In one 2016 survey of more than 1,500 Americans, 60 percent of the participants said dieting and exercise were even more effective than surgery for long-term weight loss.
Here’s the thing, though: Weight loss surgery is far and away medicine’s best treatment for severe obesity.
Related
Jewel’s journey: when everything else failed, this teen turned to weight loss surgery
The medical case for bariatric surgery has grown much stronger in recent years. High-quality studies on the long-term health outcomes of people with obesity who got surgery show, on average, that they’re able to lose dramatic amounts of weight, and even reverse or prevent their obesity-related health conditions, like diabetes and high cholesterol. A recent study in the New England Journal of Medicine demonstrated this once again. That’s why Medicaid now covers the procedure in 46 states, and so do national health systems in countries as diverse as Israel, Brazil, and Canada. It’s also why the American Academy of Pediatrics is now endorsing the operation as a “safe and effective” option for adolescents with severe obesity.
Yet out of the 20 million people who are eligible in the US, fewer than 1 percent get bariatric surgery for weight loss, according to the Obesity Society.
Why? Polling data shows that many Americans still think it’s dangerous and ineffective.
To be clear, not all weight loss surgeries are created equal: The gastric bypass and gastric sleeve operations are considered superior to the lap band, for example. And surgery isn’t for people with a few pounds to lose; it’s reserved for those with severe obesity. Even the best surgeries don’t work in some people, and can cause disturbing side effects in rare cases. But bariatric surgery’s benefits appear to vastly outweigh its harms on average, and it is shaping up to be a genuine help for people struggling through one of the most urgent health crises of our time. It’s time we started paying attention.
Weight loss surgeries work by reducing the size of the stomach and suppressing hormones related to hunger and satiety
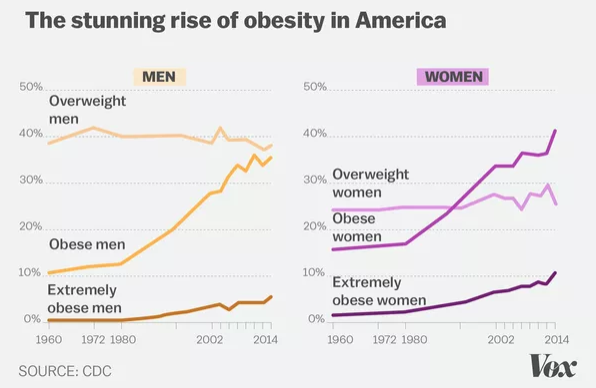
The obesity crisis in America really began to take off in the 1970s. Centers for Disease Control and Prevention estimates from 2016 now show that 40 percent of US adults and 19 percent of youth are now obese.
But long before that, doctors were searching for ways to alter people’s bodies to help them eat less food.
Jaw wiring, which involved literally wiring the jaws shut to stop people from eating, was among the early approaches. In the 1950s, researchers noticed that shortening the small intestines of dogs hampered their ability to absorb calories and caused them to lose weight. By the late 1960s, bariatric surgery was being tried in humans. Surgeons’ methods were crude at first but have vastly improved over the years. And some kinds of bariatric surgery (most recently, the lap band approach) have fallen out of favor.
Now researchers are generating longer-term data showing some of the current surgical methods can lead to dramatic and durable weight loss, and, even more remarkably, improvements in people’s long-term health outcomes.
Related
It’s easy to become obese in America. These 7 charts explain why.
The majority of bariatric procedures in America today involve the gastric sleeve and the Roux-en-Y gastric bypass. Both of these methods permanently alter the digestive tract to help people lose an average of about 30 percent of their original bodyweight (and keep most of it off — more on that later).
With the sleeve, which now makes up more than 50 percent of weight loss surgeries in the US, surgeons staple off and remove about 80 percent of the stomach, transforming the organ from a wide football shape into a slim banana (or sleeve) shape. By reducing the size of the stomach, people can’t eat as much as they used to, so they consume fewer calories.
With the gastric bypass, surgeons use staples to make the stomach smaller by creating a small pouch, which can only hold about an ounce (or walnut’s worth) of food. Next, they reconnect the small intestine to a hole in the new pouch, so food flows into the pouch, bypassing most of the stomach, and then into the latter part of the small intestine, bypassing the first half of the intestine. Like the sleeve, the surgery also restricts the amount of food people can eat, but because food no longer passes through most of the stomach, people also can’t absorb as many calories and nutrients as they used to.
But an additional reason both the sleeve and gastric bypass surgeries lead to long-term weight loss is likely because of the changes in hormones that occur after these procedures. The sleeve, and especially the bypass, seems to suppress hormones that affect hunger and satiety, like the “hunger hormone” ghrelin — something no diet will ever do.
Surgery may also reset the body’s metabolism
Another interesting possible reason for why the surgery works is that it may readjust the body’s metabolic rate, making maintaining weight loss easier.
In a 2014 study, published in the journal Obesity, researchers compared participants from the Biggest Loser reality TV show who had gone on crash diets and exercise programs to rapidly lose as much weight as possible to people who had gastric bypass surgery. (They jumped on the chance to study reality show contestants because it’s so rare to see people with severe obesity lose vast amounts of weight in real life.) The bypass surgery patients saw their metabolisms normalize within a year, to a rate that matched their new body size, while the TV show contestants saw their metabolisms slow down and stay that way — even six years after losing the weight and, on average, regaining much of it back.
Researchers suspect this is because surgery may reset the “set point,” or the body’s habit of vigorously defending a certain weight range. Once a person gains weight and keeps that weight on for a period of time, the body gets used to its new, larger size. When a person loses weight, a bunch of subtle changes kick in — to the hormone levels, the brain — increasing appetite and slowing the metabolism, all in a seeming conspiracy to get back up to that set point weight.
Amazingly, surgery seems to lower the set point, and even weaken the body’s desire to defend it. And that seems to make keeping weight off a little easier.
Not all weight loss surgeries are equally effective. The lap band surgery is not a great weight loss surgery.
The third most common weight loss procedure in America now is the lap band, though it has dramatically fallen out of favor in recent years and now only makes up about 5 percent of surgeries. The problem is the surgery doesn’t work as well for weight loss as the other procedures on offer, and it leads to lots of complications and more surgery.
Lap banding involves placing an inflatable band around the upper portion of the stomach to create a small pouch. When the lap band operation was first approved by the Food and Drug Administration in 2001, it seemed like a safe option for weight loss surgery that could be adjusted or removed at the patient’s behest. (Unlike the gastric bypass or sleeve operations, it didn’t involve permanently altering the stomach or intestines — and it could be reversed by simply removing the device.)
But long-term data suggests lap band patients lose about half the amount of weight as bypass or sleeve patients. To be clear, even losing 10 percent of one’s body weight (the average weight loss with lap banding) can improve health outcomes, but it’s a lot less than the other weight-loss surgeries. The lap band also turned out to be riskier than it seemed at first, often requiring additional surgeries.
In the best study we have on just how problematic lap band surgeries can be, published in JAMA, researchers from the University of Michigan looked at 16 years of Medicare data to see how common “re-operations” were after the first lap band procedure. These involved everything from removing the band to replacing it, fixing it, or following the initial procedure with another weight loss operation (i.e., the gastric bypass). They found 20 percent — or one in five — of the 25,000 lap band patients needed an additional procedure. That’s much higher than the 3 to 9 percent re-operation rate for the gastric bypass and gastric sleeve surgeries.
Researchers think that one reason the lap bands can fail is because they only restrict the size of the stomach, without causing the hormone and metabolic changes the sleeve and bypass do.
People who get bypass or sleeve operations lose about a third of their original bodyweight on average — and keep most of it off
In the longer-term studies of both teens and adults who got sleeve and bypass surgeries, researchers have found that people lose about a third of their original bodyweight on average and keep most of it off. So if someone weighs 300 pounds going into surgery, after a year they’ll probably weigh about 200. But not all surgeries are created equal: The lap band is dramatically less effective than the sleeve or bypass. Let’s look at the evidence.
According to a recent study, published in JAMA Surgery, researchers followed more than 1,000 adults for up to seven years and found bypass patients lost 28 percent of their original bodyweight (including regaining about 4 percent of their weight loss between three and seven years). Band patients lost only 15 percent of their original bodyweight after seven years.
In another 2016 JAMA study, looking at the four-year weight change in veterans who underwent weight loss surgery, the bypass patients lost 27 percent of their original bodyweight, the gastric sleeve patients lost 17 percent, and again, lap band patients lost 10 percent.
Another systematic review from 2015 pooled the results of many studies on different weight loss operations and found the same trend: Band patients fared the worst when it came to weight loss, and gastric bypass patients the best.
The data on adolescents who get bariatric surgery looks similar. In a 2016 New England Journal of Medicine study, researchers followed 242 adolescents who got either gastric bypass surgery or the sleeve. After three years, sleeve patients lost 26 percent of their original bodyweight while bypass patients lost 28 percent. For a 2019 paper, also in NEJM, researchers compared the health outcomes of 161 teens and 396 adults for five years after their gastric bypass surgeries. Both groups lost around a third of their original bodyweight.
Another 2017 Lancet study followed 58 American teens for eight years who underwent gastric bypass. Again, teens lost an average of 30 percent of their bodyweight. That’s a similar finding to a study out of Sweden, which tracked 81 teenagers with obesity who had a gastric bypass for five years. They lost about 28 percent of their original bodyweight.
So the data we have now suggests the surgery can be both safe and effective on average. But there’s still more researchers need to learn about the current surgical methods being used, in particular their very long-term effects on people after more than a decade or two, and whether surgery continues to mitigate the effects of obesity’s toll.
There’s some variation in how much weight people lose after surgery, and no one knows why
As with every health intervention, there are some big caveats with weight loss surgery too. One is that there’s some real variability in how people respond to it, and researchers have no way of predicting who will fare well and who won’t.
This 2018 JAMA Surgery study is a great example. The average weight loss after bypass was about 30 percent, and the majority of the study participants had lost and kept off between 20 and 30 percent of their bodyweight seven years after a bypass surgery. But there were outliers: 5 percent of the participants in the study lost as little as 10 percent of their original bodyweight, while 13 percent lost as much as 45 percent of their original weight.
While researchers can’t tell who will succeed and who will fail before a surgery, they are learning people who do well have a few things in common. In the paper, the researchers found that people who lost more weight tended to be younger when they got the surgery. They also tended to be female and white, and had a higher body mass at the start of the study.
In another 2016 paper, looking at the variables that affected weight change after surgery, researchers found that people who adopted healthier eating habits lost the most weight. So it wasn’t just the surgery that helped people; it was changes to their diet, too.
“Everyone is quite different in terms of how they lose weight and how much they lose over time,” said Anita Courcoulas, a bariatric surgery who was an author on both of these papers.
She thinks the reason is that there’s variability in the causes and subtypes of obesity among people, and that different people may need to be treated differently to get the best results. “I think the important next step is figuring out how to understand the different subtypes of obesity,” she said, “instead of treating people like they’re one homogenous group.” But we’re not there yet.
The other health benefits of surgery can be dramatic, including driving Type 2 diabetes into remission
Aside from the weight loss, the reason doctors get excited about bariatric surgery is that it seems to reduce the risk of a bunch of obesity-related diseases.
Compared to obese adults who don’t get the surgery, bariatric patients live longer, have a lower risk of cancer, have less high blood pressure, have lower rates of Type 2 diabetes, and weigh significantly less.
The JAMA Surgery study is some of the best evidence we have that these effects are durable over time. The study came out of LABS, the Longitudinal Assessment of Bariatric Surgery, a rigorous, multi-center study of bariatric patients that’s funded by the National Institutes of Health. Many bariatric studies have issues with people dropping out over time, which may bias the results. But the LABS researchers were able to follow up with more than 80 percent of the participants over seven years, which is rare in clinical medicine.
And they found that all of the patients’ health conditions — diabetes, high blood pressure, high cholesterol — were less prevalent seven years after surgery than they were before surgery. Sixty percent of the patients with Type 2 diabetes going in were still in remission seven years later. (The same wasn’t true for the group that got the lap band.)
The newest NEJM study suggests teens may see these benefits even more: They were much more likely to experience remission of their diabetes and high blood pressure than adults.
Surgery can cause complications and carry rare but disturbing side effects
Today’s weight loss surgical techniques are a lot safer than they used to be — there’s a low rate of complications that’s similar to other abdominal operations, like gallbladder surgery. But the operations still carry a 0.3 percent mortality risk and other potential harms.
The most common long-term issue bariatric surgery patients face is nutritional deficiencies. Surgeries can hamper the body’s ability to absorb nutrients, so many of the people go on to develop iron, B12, calcium, folate, and thiamine deficiencies. That’s why bariatric patients need to be closely monitored for the rest of their lives, to make sure they’re getting the vitamins they need and that they’re not developing any other health issues as a result.
Many patients also need additional surgeries for surgical complications, or “revision” operations to address problems with their original surgeries. For example, patients who got the lap band may go back for a bypass after finding out the lap band didn’t work. And between 6 and 20 percent of bypass patients need to get treatment for stomal stenosis, which is when the new connection between the small stomach pouch and the intestine narrows and doctors have to go back in a stretch it out.
The sleeve is a simpler procedure and there tend to be fewer complications requiring surgery, but they can still happen. Up to 5 percent of sleeve patients experience gastric leaks, or a hole along the staple line of the newly created stomach, which allows stomach juices to leak into the abdominal cavity. Up to 17 percent of adults who have undergone a sleeve operation are later diagnosed with Barrett’s esophagus, a complication of acid reflux disease that can lead to cancer.
Finally, some patients may opt for plastic surgery for loose, hanging skin — extra procedures that often aren’t covered by insurance.
Then there are the rare but disturbing psychological effects that have surfaced in adults after bariatric surgery, including a slightly elevated post-surgical risk of self-harm, suicide, and drug and alcohol use disorders.
Researchers still don’t understand why this happens, but they have some ideas they’re exploring. Because of the changes in the gut after bypass and sleeve operations, patients are more sensitive to the effects of drugs and alcohol.
“Any drug that peaks more quickly is more prone to abuse,” said James Mitchell, a psychiatrist who studies bariatric surgery at the University of North Dakota School of Medicine and Health Sciences. So it’s possible that bariatric surgery may make alcohol and other drugs more addicting for some people.
Junaid Bhatti, a Toronto-based researcher who has studied the link between suicide and bariatric surgery, said researchers are exploring whether this increased risk is caused by stress after surgery — the pressure to lose weight, the disappointment if you don’t. “There is a subgroup of patients that may not be able to adjust well to the restrictions that come after surgery and if they have any previous mental health issue that may be provoked because of that stress following surgery,” he explained. Or maybe there’s some other yet-to-be-discovered physiological change after surgery that explains it.
These two effects — the drug abuse and mental health issues — may work together in dangerous ways, Mitchell added. “When people are intoxicated, they are disinhibited. If they are depressed and thinking about suicide, that’s not an uncommon time for them to act. So those two things may converge in a bad way that needs to be looked at in more detail.”
There’s another nonmedical — but important — side effect of going under the knife for weight loss surgery: experiencing a change in relationship status. A study out of Sweden, published in JAMA Surgery, found people with spouses or live-in partners were more likely to separate or divorce after surgery compared to control groups who didn’t get surgery, while single patients were more likely to get into a relationship.
The new NEJM paper found these serious complications — nutrient deficiencies, self-harm, additional operations — may be more common in teens than adults. So there’s an urgent need to understand them.
Bariatric surgery isn’t necessarily cost-saving. But it’s cost-effective.
Then there are the important cost considerations. Without insurance, bariatric surgery can cost more than $20,000. And that doesn’t include the cost of additional operations and follow-up care. So bariatric surgery isn’t necessarily going to make a big dent in America’s obesity-related costs, which add up to about $210 billion per year.
“The expectation is bariatric erases these obesity-associated costs,” said David Arterburn, an obesity expert at Kaiser Permanente Washington Health Research Institute, “but because of the small complication rate and because complications are expensive — requiring hospitalization, reoperation — my take on the literature is that there’s no cost savings that happens from bariatric surgery.”
The average patient with severe obesity uses between $5,000 and $10,000 in medical care per year, he said. Out of those total costs, about a third are associated with their obesity. The rest is related to other problems, like arthritis or high blood pressure that’s brought on by aging. Bariatric surgery can help cut the obesity-related costs, but not necessarily these other costs or the follow-up.
Even so, bariatric surgery is considered “cost-effective,” meaning it’s as effective or better than similarly expensive interventions.
“Cost-effective treatments are considered somewhere between less than $50,000 to $100,000 per quality-adjusted life year saved [QALY],” explained Scott Kahan, director of the National Center for Weight and Wellness and a professor at George Washington University. “Bariatric surgery is in the range of $50,000 per QALY.” By comparison, annual Pap smear screenings are estimated at $800,000 per QALY, kidney dialysis $50,000 to $100,000 per QALY, and spinal fusion $250,000 per QALY.
“This is right in that sweet spot of we are spending a reasonable amount of money and getting a reasonable return,” Kahan added.
Researchers think the surgery could be even more cost-effective in adolescents — not only because they’ll likely experience greater health gains than adults (since they’re young and many of their health problems are more reversible), but also because they’ll be better positioned to contribute to the economy if they’re unencumbered by severe obesity.
People who want surgeries aren’t always able to get them
Again, fewer than 1 percent of people get a bariatric surgery for weight loss. And researchers and obesity experts think there are several reasons for that.
A lack of understanding about obesity and obesity-related stigma may hold both doctors and patients back from considering surgery. “There’s an attitude that people are at fault for their obesity, that it’s failure or personal responsibility,” said Joe Nadglowski of the Obesity Action Coalition, a membership organization for people with obesity. “Not only is having obesity something you’re stigmatized for, but if you need a medical intervention, there’s a stigma around needing help to deal with it.” So doctors may think patients can exercise their way out of the problem, and patients may feel they should be able to, too.
In a seminal 1991 study, researchers asked patients who had lost about 100 pounds after surgery to choose between regaining their weight or maintaining their new body size at the cost of living with another disability. The patients opted for deafness, blindness, heart disease, even losing a limb, instead of returning to their morbid obesity.
Insurance coverage is “all over the place,” Kahan said. Though many providers cover the surgery, copays can be high, and insurers often don’t pay for follow-up operations or plastic surgeries that are needed later. “Even when there is coverage, it’s quasi-coverage,” he added. “Copays can range from hundreds of dollars to over $10,000 in some policies. For some patients, surgeries are exempt from out-of-pocket maximums.”
Many doctors still don’t know the basic requirements for a bariatric surgery recommendation and may not be referring patients who could benefit from surgery, he added. In a 2007 survey of nearly 500 doctors, 91 percent referred their severely obese patients to exercise, with diet following closely behind. The least-recommended weight loss treatment was bariatric surgery, prescribed for only 15 of the doctors’ morbidly obese patients.
We can’t cut our way out of the obesity epidemic
Almost all the researchers I spoke to for this story said they hoped to one day find a pill that could do for obesity what surgery does. But until then, surgery is the best thing we have for the treatment of obesity. That doesn’t mean it’s the answer to the obesity epidemic, however.
“The obesity epidemic did not occur because we don’t have enough surgery,” said National Institutes of Health obesity researcher Kevin Hall. “The obesity epidemic occurred because the food environment has changed remarkably.”
There’s no question that our food landscape has increased the opportunities for obesity-related genes and traits to express themselves. Preventing future obesity cases will require making it easier for people to eat healthfully and be more active. But there’s still the problem about what to do for the people who are struggling with severe obesity right now.
“[Surgery] is an incredibly valuable tool right now for treating adults with [severe] obesity,” Hall added, “but we’re not going to cut our way out of the obesity epidemic.”
Sourse: vox.com






