
In the United States, around 735,000 people each year have a heart attack. In all, heart disease (and its complications, including heart attacks) kills 610,000 a year here, making it the leading cause of death in America and worldwide.
Preventing heart disease is a huge public health challenge. And right now doctors have good, but limited, options for finding out who is at greatest risk for it.
Doctors know that about half the risk for heart disease comes from lifestyle choices: how much, and what, a person is eating, how much alcohol they drink, if they smoke.
The other half is related to genetics, and it’s much harder to assess. You can ask a person about their family history of heart disease and can check for high blood pressure and obesity, which are also related to genetics. But up until the recent explosion in genetic science, it was hard to probe the genes themselves.
Related
How scientists are learning to predict your future with your genes
Last week, in the journal Nature Genetics, researchers at Harvard University and the Broad Institute published evidence that they can check out 6 million spots in a person’s genome to assess their risk for developing coronary artery disease, when the main blood vessel supplying the heart with oxygen gets clogged with plaque. It’s a precursor to a heart attack, when a clot cuts off blood flow to the heart, starving it of oxygen.
In the study, people who carried the greatest number of genetic variants suggestive of heart attack risk were three or more times likely to develop coronary artery disease than controls. The researchers argue that with this test, about one in 12 people could be identified as having a higher risk of heart attack based on their genetics alone.
“If you told me there was a genetic score that could identify 8 percent of the population with more than a threefold risk, I’d say, that’s amazing,” Robert Yeh, a cardiologist at the Smith Center for Outcomes Research in Cardiology, who was not involved in the study, says. Currently, the best commonly available genetic test for heart disease risk — which looks for a single gene linked to high cholesterol — can only detect increased risk in 0.4 percent of people.
“The big takeaway is that we can now capture the inherited component to heart attack risk with a single number,” Sekar Kathiresan, the Massachusetts General Hospital cardiologist and geneticist who led the study, says. With this new tool, Kathiresan hopes doctors could put those people at higher risk on cholesterol-lowering medications (statins) at an earlier age, or more easily persuade them to make lifestyle changes to lower their risk.
The new tool here is called a polygenic risk score, which you can think of as a tally of the tiny changes in your genome that are correlated with risk of developing a disease.
In the coming years, you’re going to hear a lot more about them. These scores, while increasingly helpful in some areas of medicine, come with a lot of caveats. Indeed, when you dig a bit deeper into this latest Nature Genetics paper, you find there’s a lot more work to do to validate polygenic risk scores for heart disease, so they will be useful and relevant to people around the globe. For one: This study was exclusively conducted with subjects in the UK of white European background. The predictions derived from this group do not necessarily transfer over to another. For this and other reasons, scientists skeptical of polygenic risk scores say they are not yet ready for the clinic — and wonder if they will ever be.
At the same time, it seems likely these polygenic risk scores are going to change the way we think about our health and our medical decision-making.
What’s a polygenic risk score?
Over the past decade, medical researchers have realized that our risk for many common conditions like heart disease and diabetes are not influenced by just one gene, or even a small handful of them. Instead, studies analyzing huge numbers of sequenced human genomes have found that there are hundreds of genes that work in constellation influencing our risk for diseases.
DNA is the recipe for our biology. But it turns out that recipe looks something like an M.C. Escher drawing, with a huge number of genes influencing life outcomes in hard-to-understand, hard-to-follow, interconnected ways.
That is, there can be hundreds of interrelated spots in the genome that are correlated with a person’s risk for heart disease, or raising or lowering their height by a millimeter. Scientists are getting better at identifying these spots in the genome that confer risk and are now trying to figure out if tallying up these genetic changes — in what’s known as a “polygenic risk score” — is useful in trying to predict, and prevent, disease. (They are also calculating them for behavioral traits like educational attainment.)
In developing polygenic risk scores, in many cases, genetics researchers often don’t know what the underlying genes do. All they know is that these genes are correlated with — which does not mean cause — the disease. “It’s pretty mindless,” says Cecile Janssens, an epidemiologist at Emory University who is critical of the hype of polygenic risk scores.
Proponents of polygenic scoring, though, argue that you don’t need to know what the genes are doing to make predictions off them.
“It’s all about getting a predictor and then repeating it in other groups,” Kathiresan says. “At the end of the day, I could just call it a magic number generator. It doesn’t exactly matter how I’m getting there, as long as it works in other groups equally well.”
That’s what happened in this latest paper. A polygenic risk score derived from huge genome-wide association studies predicted heart attack risk in nearly 300,000 people in the UK. (Read more about how scientists come up with polygenic risk scores here.)
How good is the prediction?
Because each change in the genome — called single nucleotide polymorphisms, or SNPs (pronounced “snip”) — confers such a tiny change in risk, adding more and more of them to the risk score yields diminishing returns. “We see this trend already for years — every new SNP that we discover has a smaller effect than we knew already,” Janssens, says.
In the recent Nature Genetics study, she points out, when the researchers increased the number of SNPs in their risk model from 74 to 6 million, the predictive power of the test only increased by a smidgen. Most of those SNPs have a predictive power of approximately zero.
Here’s a chart showing where the polygenic risk score for coronary artery disease matters most. Polygenic scores, like so many human traits, are normally distributed, meaning they follow the pattern of the bell curve. But a person’s risk for coronary artery disease really only starts to increase if they have the very highest number of SNPs that are correlated with heart disease risk. The top 8 percent of the participants had a three times greater risk of heart disease. The top 0.5 percent had five times the risk.
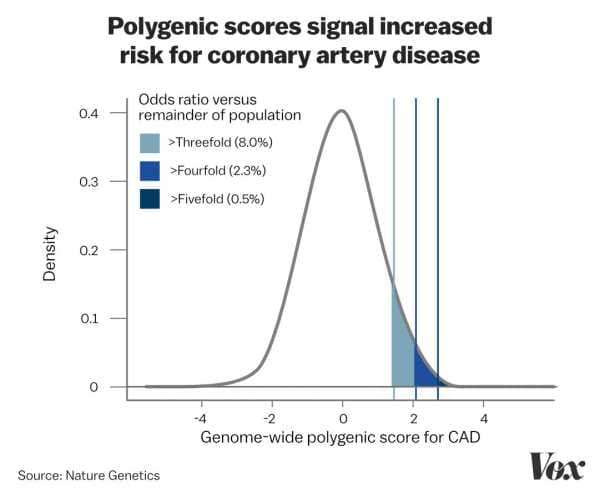
There are many caveats to this risk prediction, which the authors of the study acknowledge. One is that it’s currently unclear if predicting heart attack risk in this manner provides an additional benefit to the risk models derived from asking people simple questions about their lifestyle and family history. The researchers suspect it does, but they didn’t set up their study to test this question.
Another is that this risk model was developed and tested solely on people who had donated their medical and genetic information to the UK Biobank, which contains only genetic data of people of white, European ancestry. The predictive power of these tests is expected to diminish in people of African ancestry, Asian ancestry, and so on. Genetics researchers will need to repeat polygenic risk studies with data from these populations if these predictions are truly going to be useful and equitable.
And yet one more: We shouldn’t take it for granted that intervening with early medication or lifestyle changes for the people at highest risk will make a difference in lowering their risk. Other studies have found that people with higher genetic risk scores for atherosclerosis tend to receive a stronger benefit from statins. But the question needs further testing.
All that said, Yeh, the research cardiologist, says there’s still a lot of optimism around these scores. Current risk factors for heart disease, like high blood pressure or family history, don’t always help single out who truly is most at risk.
“The majority of being who develop coronary artery disease are not people who have a multitude of cardiac risk factors,” Yeh says. “About half of people have just one risk factor, high blood pressure alone. People like that, although they only have one cardiac risk factor, sometimes none, they wouldn’t think of themselves of [having] a very high elevated risk for coronary artery disease.”
A genetic risk factor could help narrow it down.
We’re going to start seeing more and more polygenic tests for disease risk
Polygenic risk scores, says Eric Topol, a cardiologist and geneticist with Scripps Research, “are going to take hold in common medical practice. It’s a matter of when, not if.”
And they’ll be used for conditions outside of heart disease. Indeed, in the latest Nature Genetics study, the researchers also calculated risk scores for diabetes, atrial fibrillation (irregular heart rhythm), inflammatory bowel disease, and breast cancer. The genetic tests for these conditions found fewer people at elevated risk than the tests for heart disease. And not every test will be equally predictive.
Kathiresan points out that while only 8 percent of the study participants were singled out for elevated risk for coronary artery disease, about 20 percent of all the participants were flagged as having elevated risk for at least one of the diseases listed above.
And while these scores are now being generated for all kinds of health and behavioral issues, medicine isn’t really ready to implement them. Huge questions remain. For instance, while it’s possible to do a genetic risk assessment of an infant, or even an embryo, does it make sense or is it even ethical for new parents to learn their embryos or newborns are at a threefold risk for heart disease?
Doctors will also have to think long and hard about how they discuss these kinds of risks with their patients. Scoring in the 70th percentile of risk for coronary artery disease may sound scary, but it won’t increase a person’s chances of getting that disease by all that much.
There are also likely to be unintended consequences of giving patients a new health metric to fear. Consider what happened with cholesterol, a risk factor for heart disease that people began being commonly tested for in the 1980s. Fear of cholesterol came to inspire low-fat food trends. Those dietary trends made food companies money, but they didn’t necessarily make people healthier, especially as many of the foods marketed as low-fat were still loaded with sugar.
What happens when some huckster starts selling vitamins to complement a polygenic risk score, or some other forms of woo? (Currently, you can buy a customized diet guide based on a sequencing of your DNA.) There’s a lot of education that needs to happen here to prevent genetic risk prediction from becoming genetic astrology.
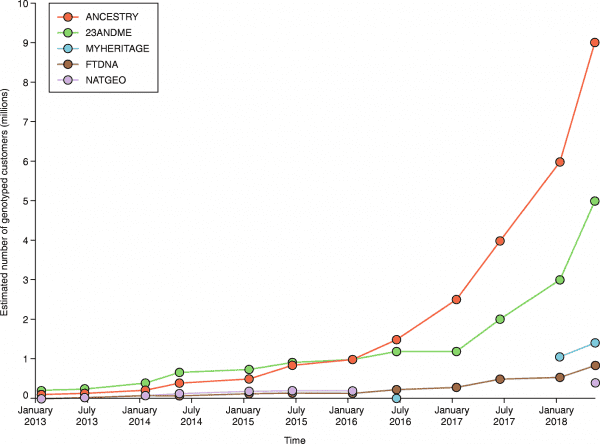
For now, aside from a polygenic risk score for breast cancer, these tests don’t yet exist in the clinic. But they’re going to get easier and easier to discover on your own. If you have your genetics data from a commercial company like 23andMe, you can upload it to a number of sites on the internet to see your risk scores for a slew of traits and diseases. Kathiresan’s team is hoping to build a free tool for people to assess their coronary artery disease risk in this manner.
Here’s a reasonable fear: It’s going to be hard for consumers, without much input from doctors, to know when the risk scores matter and when they do not. Heck, you can currently take a genetics test for intelligence that really won’t tell you anything valuable. It’s possible to develop polygenic risk score for loneliness, baldness, marital status, or really any human trait that is even vaguely influenced by genes. It takes more information — like odds ratios — to know whether those scores really matter in your life.
It will also be hard to know what to do to diminish risk. A high polygenic score for breast cancer might mean a woman wants to make more frequent mammogram appointments, Janssens says. But the current recommendations for people at higher risk of heart disease are things everyone should be doing: living a healthy lifestyle free of tobacco.
“I actually think there’s going to be a whole [medical] field that emerges, kind of like radiology emerged in 1900 with the invention of X-rays,” Kathiresan says, “where [doctors] are basically interpreting that genetic information for medical risk.”
That field needs to start up soon, because there’s a lot more coming.
Sourse: vox.com






