We don’t talk much about chlamydia, gonorrhea, or syphilis, in part because it can seem like they’re not big health issues anymore. But it turns out more and more Americans may be quietly suffering from these once nearly eliminated STDs.
According to a new report from the Centers for Disease Control and Prevention, there were nearly 2.3 million cases of chlamydia, gonorrhea, and syphilis reported in the United States in 2017 — the highest cumulative number ever recorded, and one that surpassed a 2016 record high.
The leaps in cases over the last few years are truly eye-popping. Between 2013 and 2017, the rate of:
- Gonorrhea increased by 67 percent to 555,608 cases
- Syphilis increased by 76 percent to 30,644 cases
- Chlamydia increased by 22 percent to 1.7 million cases
To appreciate just how astonishing the trends are, consider that as recently as a decade ago, these STDs were at historic lows or near elimination, with more and better screening and diagnostics to help identify cases and get people into treatment.
Syphilis can show up on the body in sores and rashes. Gonorrhea and chlamydia can lurk with no symptoms. They’re all generally easy to cure with a timely antibiotics prescription, but when left untreated, they can lead to infertility or life-threatening health complications. That’s what makes screening and access to health care so important.
The increase in cases between across all three diseases was significant, and represents changing disease dynamics.“We are sliding backward,” said Jonathan Mermin, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, in a statement. “It is evident the systems that identify, treat, and ultimately prevent STDs are strained to near-breaking point.”
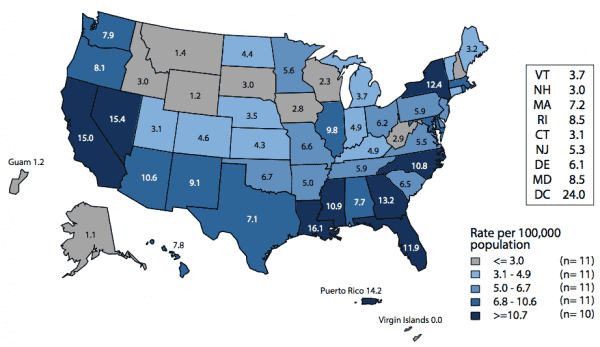
African Americans and men who have sex with men have traditionally been the populations most plagued by gonorrhea and syphilis (and they’re still disproportionately affected). But other groups are now catching up too, especially women and babies in contracting syphilis.
So what’s behind the spread of these diseases here? There’s no single explanation. Like most health trends, it’s complicated. But here are a few ideas, according to experts:
1) There’s been a rise in condomless sex among men who have sex with men: Gay, bisexual, and other men who have sex with men are generally more at risk for STDs than women and men who have sex with women only. (The majority of new syphilis and gonorrhea cases occurred among men, and in particular, men who have sex with men.) And there’s been some concern about a shift toward riskier sexual behaviors in this group — like not wearing condoms — that may be contributing to the rise in STDs.
The reason for this shift has been explained by everything from the success in treating HIV (and therefore making sex less scary) to the advent of PrEP (pills that can prevent HIV). A systematic review published in the journal Clinical Infectious Diseases found that some PrEP users are having more risky sex — and are being diagnosed with more sexually transmitted infections.
HIV and syphilis are also interlinked: Some half of men diagnosed with a new syphilis infection also have HIV. And as these diseases spread in particular populations, like men who have sex with men, there’s a greater risk of them moving even further.
“The fear, which I share, is that we won’t contain syphilis among men who have sex with men,” Matthew Golden, director of the Public Health for the Seattle and King County HIV/STD control program, told Vox in 2017. “And if the epidemic in men who have sex with men gets big enough, which is what is happening, there are enough people who have sex with both men and women that it won’t be possible to contain it.”
2) STDs are spreading more broadly and into populations that weren’t traditionally affected — like babies: A 2017 CDC report on STDs in America showed that more women are getting syphilis these days, and they’re passing it to their babies. When an expectant mother is infected with the disease, and goes undiagnosed and untreated, the bacteria can get into her bloodstream and move through her placenta to her baby. Congenital syphilis is associated with serious health consequences, like stillbirths and neonatal deaths.
In 2016, there were 628 cases of congenital syphilis, an increase of 27.6 percent from 2015 — and that number includes 41 related deaths. According to the CDC, much of the rise was driven by increases in cases in the Western US. Between 2012 and 2016, Western states saw an astounding 366 percent rise in congenital syphilis.
The large increase has to do, in part, with the fact that many Western states have recently had few syphilis cases in women. “We were starting from almost nothing [in Washington],” said Golden. But that’s changing, and with more women getting the disease, their babies are at risk too.
3) With the rise of dating apps, sex is more readily available and more anonymous — and that makes it harder for health investigators to track outbreaks: Health experts increasingly view apps and sites such as Tinder, Grindr, and OkCupid as enablers of high-risk sex, helping people meet and hook up more efficiently than ever before. The impact of these sites is so profound they are also transforming the way health officials track and prevent outbreaks.
“We used to think about what we can do with bathhouses and sex clubs to make sure people’s risk was reduced,” said Dan Wohlfeiler, director of Building Healthy Online Communities, a public health group that works with apps to support STI prevention, told Vox in 2017. These places, after all, had become important meeting points for men who have sex with men — the group most affected by the HIV epidemic.
Today, the public health focus has shifted to “digital bathhouses.” Wohlfeiler said, “Now that dating sites and apps have become so common, we know we need to work with them.”
But many of the major dating networks don’t want to be involved in STD prevention, nor have they acknowledged the impact they’re having on public health, health experts told Vox.
4) The numbers may be higher because we may be better at detecting cases in some groups: The rise in chlamydia — which overwhelmingly causes no symptoms but can lead to infertility in women — may be an artifact of better detection and screening. The CDC keeps finding that rates of chlamydia are highest among young women, the group that’s been targeted for routine chlamydia screening. So an increase could just mean more testing.
5) Cuts to public health funding mean fewer STD clinics: Public health in the US — which includes operating STD clinics where people can get tested and into treatment — is historically underfunded. (As of 2012, only 3 percent of the health budget went to public health measures; the rest went mostly to personal health care.) And since the global financial crisis, public health funding has really taken a battering. There are 50,000 fewer public health jobs since 2008, and many STD clinics have had to reduce their hours or shut down.
STD clinics were a traditional safety net for people with these diseases. If those clinics continue to be harder to reach or vanish, finding and treating STDs will become even more difficult — and the diseases will continue to spread.
So in some ways, the STD increases across the country may have less to do with a changing sexual landscape, and more to do with more limited access to sexual health care. With Trump’s proposed public health budget cuts, the problem may be poised to get worse.
“It’s not a coincidence STDs are skyrocketing — state and local STD programs are working with effectively half the budget they had in the early 2000s,” said David Harvey, executive director of the National Coalition of STD Directors, in a statement today. “If our representatives are serious about protecting American lives, they will provide adequate funding to address this crisis. Right now, our STD prevention engine is running on fumes.”
Sourse: vox.com






