How your body will try to save you from Covid-19
Covid-19 immunity — antibodies, serological tests, reinfection, and immunological memory — explained.
By
Brian Resnick and Umair Irfan
Apr 23, 2020, 1:00pm EDT
Share this story
-
Share this on Facebook
-
Share this on Twitter
-
Share
All sharing options
Share
All sharing options for:
How your body will try to save you from Covid-19
-
Reddit
-
Pocket
-
Flipboard
-
Email
Part of
The Vox guide to navigating the coronavirus crisis
The Covid-19 coronavirus meets its most formidable foe the moment it enters the human body.
The immune system is waiting, ready for action, and it determines who dies and who survives. It is why the vast majority of the infected have recovered from the disease.
Yet one of the most important unknowns is why some people’s immune systems are up to the task of clearing out the virus while others are sluggish or overreact, leading to death. Just as vexing:
- How do we know for sure if a person is immune to Covid-19 after infection?
- What percentage of the US population will be immune after this first wave of infections is over?
- Will immunity last over time, or will it fade?
- Can a vaccine provide immunity and stop the pandemic?
It’s helpful in thinking through these unanswered questions to understand how the immune system works (collectively and in individuals), how immunity testing works, and how immunity to similar viruses changes over time. It’s also comforting to know that if you get Covid-19, your body will try very, very hard to save you. And if it doesn’t, it could be because it tried too hard.
So here is a guide to the immune system: antibodies, serological tests, reinfection, and immunological memory, explained.
Your immune system is like a beautifully complex orchestra. It plays two movements.
The first thing to know about the immune system is that it is not simple. At all.
A huge array of cells and chemicals your body produces work in concert to clear a foreign invader from your body. “There’s a lot of elegance to this whole system,” Akiko Iwasaki, an immunologist at the Yale School of Medicine, says. “It’s like an orchestra.” All these cells and chemicals have to work in concert — each with a different part to play — to defeat the virus.
A viral infection begins when a virus enters a cell of your body. In the case of Covid-19, which is transmitted mostly by respiratory droplets, maybe that takes place somewhere in the lining of your nose or in the area of your lungs directly in contact with the air you inhale.
The virus then attaches to a cell — via a protein on the cell’s surface called ACE-2 — and lets itself in.
There, it begins to wreak havoc. The virus hijacks the cell’s machinery to make copies of itself. Those copies break out of the cell and then spread around your body. The copies enter more of your cells, make more copies, and so on. This is going viral, in the literal sense, and it’s a process your body works furiously to stop.
If the immune system is an orchestra in concert, it can be broken down into two movements.
First, the opening: the innate immune response. This is the base-level protection you have to defend against infections — even those your body has never seen before.
Iwasaki explains that every cell of your body has something of its own immune system in miniature. Your cells “have a mechanism to detect virus infection,” she says. Every cell is looking out for telltale genetic signs of viral replication. Once that’s found, your cells “start secreting these cytokines [signaling molecules] to tell the neighboring cells that there’s a viral infection,” she says. “It will signal that cell to make a lot of antiviral proteins. Every part of the viral life cycle is targeted by hundreds of genes that are induced by this.”
“There’s a lot of elegance to this whole system. It’s like an orchestra.”
The innate immune response will then try to stop the virus in its tracks there, but it can fail, as we know. Viruses — those sneaky bastards — have evolved ways to counter this initial response. The viruses “might encode proteins that degrade some of these signaling molecules,” Iwasaki says. “Even though we have this amazing system, viruses try to circumvent it.”
If the innate immune system can’t get rid of the infection, the second movement in this orchestration begins: the adaptive immune system. It has a vast array of instruments, each tuned to a specific task.
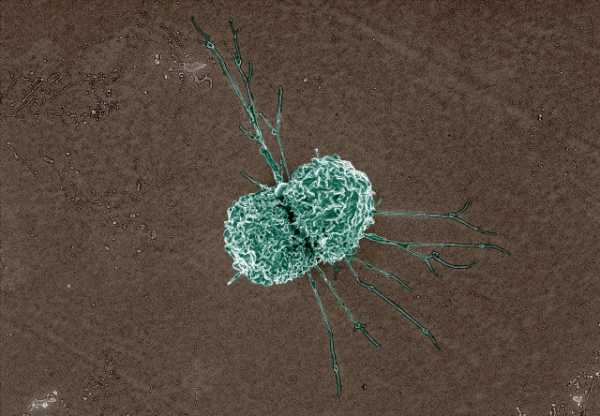
There are dendritic cells, which act as messengers from the innate immune system and tell the adaptive immune system which viral proteins it should seek out and destroy. There are killer T-cells, which hunt down and kill cells that have been infected. There are helper T-cells, which stimulate killer T-cells and recruit yet another class of cells called macrophages to gobble up infected cells, and they also stimulate B-cells, which bring this whole concert to a crescendo.
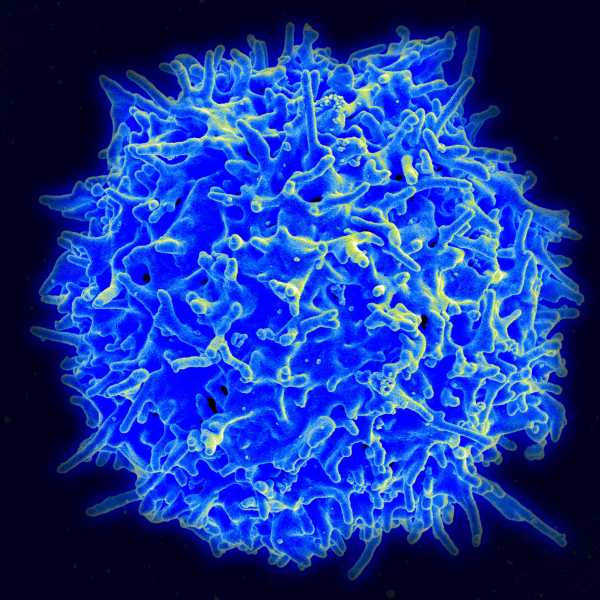
B-cells are critically important because they produce antibodies. These are little proteins that bind, specifically, to a single distinct part of a virus or pathogen and make it unable to hijack your cells. Antibodies can also identify invaders for other immune cells to destroy, and they can mark infected cells for destruction before a virus can burst out. And after an infection fades, the antibodies that linger can prevent the same virus from rising again.
But this process takes time.
“When you first get infected with SARS-Cov-2, it usually takes anywhere from 10 to 14 days to make antibodies that are effective,” says Vineet Menachery, an immunologist who studies coronaviruses at the University of Texas Medical Branch. “That immunity actually peaks between four and eight weeks after you’ve been infected. The antibodies are really powerful at that point.”
It takes a long time because an antibody has to be unique for the virus it’s trying to protect against. It takes a while — and some trial and error — to both build an antibody that can perfectly bind to the contours of the virus and to produce millions of copies of that antibody. The process isn’t simple, but you can be in awe of it, like you can be in awe of a timepiece constructed from hundreds of delicately selected parts. “I teach an entire semester course on this,” Iwasaki says. This is the delicate process that a vaccine is trying to replicate artificially.
This antibody construction process can backfire, however. In some cases, antibodies bind to the virus, Iwasaki explains, and instead of blocking the virus, they’re taken up by white blood cells. Those white blood cells then go haywire, producing molecules called cytokines. Ordinarily, these chemicals promote inflammation throughout the body.
Inflammation is something that makes us feel sick, but it also helps us survive. “People often think of swelling when they think of inflammation,” Angela Rasmussen, a Columbia University virologist, says. Swelling occurs because cells from your immune system are rushing into the site of the infection. These immune cells “have to get out of your blood vessels,” she says, in order to corral the infection. “It’s a lovely process called rolling extravasation,” she says. “Your tissue gets inflamed because the balance of fluid is being changed.”
But sometimes, so many cytokines are released that they trigger white blood cells to turn against healthy cells. That can then lead to organ failure and death. “And that ultimately makes the disease as bad as it is,” Iwasaki says.
It’s unclear why a “cytokine storm,” as this reaction is called, might impact some people severely and not others, though there are indications that aging is a factor, as are underlying conditions like high blood pressure and diabetes. Researchers are also now looking for genetic clues to see who is most at risk. Thankfully, though, doctors do have some insights into how to treat this overreaction.
This whole orchestra ends when the immune system neutralizes all the virus in the body. That doesn’t always mean the virus is purged; many viruses can linger in a latent state in the body without reproducing or causing symptoms. These latent viruses can flare up when the immune system is weakened, causing opportunistic infections. At the same time, you’ll be left with antibodies circulating in your blood.
But for reasons scientists don’t quite understand, for some infections — and notably, in other types of coronavirus infections — antibody levels can wane over a period of years.
How do we know if someone is immune? There are two main tests.
So how do doctors and scientists know if this process has been successful? How can they know if someone is now immune to the virus that causes Covid-19?
They test for it.
In particular, blood tests, also known as immunity tests or serological tests, can reveal who possesses antibodies to the virus. Deploying these tests will help answer a lot of questions. Most basically, it can help a person know if they have had Covid-19.
On a larger scale — if deployed in well-designed studies — serological tests could reveal the complete picture of the pandemic. They can also help scientists answer basic questions like:
- How many people infected with the disease die?
- What percentage of the population has been infected?
- Who, and how many, may have spread it without knowing it?
Serological tests could also potentially allow people who have immunity to return to work. That could be a huge boost to front-line health workers who may have been exposed to the virus but are desperately needed back in action.
Just finding the antibodies isn’t always enough, though. Scientists also need to do additional tests to make sure those antibodies are potent.
“There are two main types of antibody tests,” Menachery explains. The first just looks for antibodies and can be completed in a few hours. This is called an ELISA test (short for Enzyme Linked Immunosorbent Assay). And it doesn’t provide the most complete picture of immunity.
The second test is more involved, and rarer. It’s called a serum neutralization test, and it takes a few days to process. It not only looks for antibodies, it then exposes those antibodies to a virus in a cell culture to see how effective the antibodies are in stopping the virus.
Ideally, scientists will correlate the two tests and figure out which concentrations of antibodies confer the highest level of immunity. “This work is ongoing,” Menachery says. It’s still not known what levels of antibodies are needed to have lasting, protective immunity. (What also remains to be shown: that the presence of antibodies also means you can’t give the virus to someone else.)
These tests are useful, but they don’t answer everything. As noted earlier, it takes days, if not weeks, for the body to produce antibodies. So a negative antibody test doesn’t mean the virus isn’t present. And since antibodies are produced during an infection and linger after it’s cleared, a positive antibody test doesn’t mean that the virus is no longer active.
Confirming whether someone can still spread Covid-19 requires a separate genetic test like an RT-PCR test that detects the active virus.
Your levels of antibody can wane over time, but it doesn’t mean you are defenseless
Even if people do become immune, “one thing we don’t know about still is how long that immunity would last,” Rasmussen says. “And that’s unfortunately not something we can determine until we wait months or years in the future, and test again and see if those antibodies are still there.”
For reasons scientists don’t quite understand, for some infections, your immunity never wanes. People who are immune to smallpox, for example, are immune for life: Antibodies that protect against smallpox have been found as long as 88 years after a vaccination.
Less reassuring here is that scientists have observed antibody levels to other coronaviruses (there are four coronavirus strains that infect people as the common cold) can wane over a period of years. A few weeks after an infection, antibody levels will be at their highest. But “a year from now, that number is likely going to be a little bit lower, and five years from now it’s likely to be potentially a lot lower or a little bit lower, and we don’t know the factors that change that,” Menachery says.
However, even if you lose the antibodies, it doesn’t mean you are again completely susceptible to the virus. Yes, none of this is simple.
There have been a few experiments where volunteers were willingly exposed to a coronavirus strain that produces a common cold. These studies show it’s common for the antibodies to these other coronavirus strains to decline after a year or so.
Related
“Human challenge trials,” where healthy volunteers would be exposed to Covid-19, explained
“The majority of people that don’t have serum neutralizing antibodies [i.e., antibodies that take out the virus], they get infected again, but they didn’t get that sick,” Menachery says. You couldn’t do this type of test for Covid-19, he adds; it’s too dangerous.
There have been reports of a few patients out of China who had mild symptoms of Covid-19 who did not have detectable neutralizing antibodies after recovery, though they did have another form of antibody that binds to the virus. “It’s unclear whether they have protective immunity,” Nature reports. Yes, there is more than one type of antibody, and they do different things, because none of this is simple.
Luckily, even if your antibodies against a coronavirus decline, your body has a backup plan.
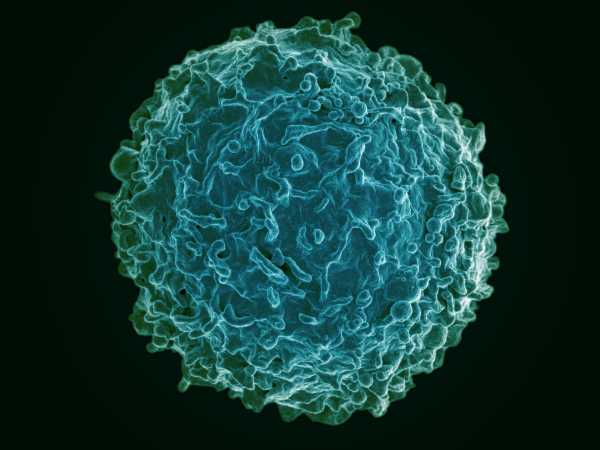
Certain types of B-cells — recall, these are the ones that make antibodies — become memory B-cells. These save the instructions for producing a particular antibody, but they aren’t active. Instead, they hide out — in your spleen, in your lymph nodes, perhaps at the original site of your infection — waiting for a signal to start producing antibodies again.
For reasons scientists don’t quite understand, for some infections, your immunity never wanes
With the memory B-cells in reserve, instead of waiting two weeks or more to get antibody production going, “you’ll only have to wait maybe two or three days,” Menachery says. “So that means, yes, you can get infected again, but you may not even know you’re sick. If you do get sick, maybe it’s a very minor infection.”
Generally, he says, the more severe your infection, the more antibodies your immune system will produce, and the longer they’ll stay in your bloodstream post-infection. So, he says, “there is some concern that if you had a mild infection that your level of protection may not last long.”
You may have seen some reports of people testing positive a second time for Covid-19 after recovering. The experts we spoke to say these reports are likely due to flaws in testing. “I think the risk of being infected more than once from SARS-CoV-2 is nil,” says Gregory Gray, an infectious disease epidemiologist at Duke University, in an email.
That may be because as you progress in the illness, the testing for Covid-19 becomes more inconsistent.
“Often at the time that virus diseases present themselves, it’s fairly far into the replication of that virus in that person,” says Diane Griffin, a professor of microbiology and immunology at the Bloomberg School of Public Health at Johns Hopkins University. “Many symptoms of virus disease are actually manifestations of the immune response to the disease. Often things are starting to get better at the time you’re starting to figure out someone even has a virus infection.”
At least in the short term, it’s probably more the case that the people who have tested positive after recovering haven’t completely cleared the virus from their system or that a prior negative test was inaccurate.
Over the long term, the immune system itself becomes less effective with advancing age. And as people get older, they can acquire more chronic illnesses that can hamper the response to a virus, even if it’s one the immune system recognizes. It will be years, though, before scientists can understand what aging means for immunity to Covid-19.
Why widespread serology testing isn’t going to necessarily save us
The Centers for Disease Control and Prevention is now conducting serological surveys for Covid-19 antibodies in several places across the US.
It’s an attempt to figure out who was previously infected with the virus, particularly if they never exhibited symptoms. A survey like this can show the actual background rate of infection and answer critical questions like what proportion of people have been infected without showing symptoms and where the virus has spread in a population, and quantify the overall rates of severe complications. Knowing these variables can help health officials better target interventions.
Many people who may have been infected also want to know if they are immune so they can safely leave lockdowns. Countries like Germany are even considering granting immunity passports so individuals can return to work.
Such testing could make a difference in a handful of cases, like for doctors and nurses who were infected or may have been exposed but are desperately needed back in action. But serological testing is unlikely to be a wholesale solution to reopening the economy.
Again, scientists are still uncertain about the robustness and duration of immunity that a Covid-19 infection confers, so a positive antibody test at this point doesn’t guarantee that one can safely end social distancing measures. If immunity does fade after a year or two, the same person could be vulnerable to reinfection.
Meanwhile, to reopen schools, shops, and offices across the board, large numbers of people would have to have immunity. Without a vaccine, that would mean that the virus would have to infect vast swaths of the population, in the process sending thousands to the hospital and to their graves. That is exactly what measures like lockdowns and social distancing are trying to avoid.
While this outbreak has been ghastly, it has not been so bad as to bring about herd immunity in any quick time frame. There have been some — imperfect — serological studies that suggest the virus has infected more people than previously estimated. But even if true, the studies don’t mean we’re anywhere close to achieving herd immunity.
So it’s unlikely that immunity can be a benchmark for when it’s okay to go back to normal across the population, and even in individual cases, it requires careful consideration of risks and benefits.
Getting infected with Covid-19 isn’t the only way to become immune to the virus
For those who have not yet contracted the virus, the main form of protection from Covid-19 right now is prevention. But there are several options scientists are studying that could help those who were never infected fend off the illness.
Chief among them is a vaccine. A vaccine can take various forms, including a weakened version of the virus itself, a small piece of the virus, or genetic material that prompts the immune system to manufacture antibodies to the virus.
Developing a vaccine for SARS-CoV-2 would be the ideal solution to the Covid-19 pandemic since it’s a form of prevention that would also hasten the end of costly measures like lockdowns, quarantines, and social distancing.
But it’s a time-consuming approach. Many experts estimate that it will take at least a year to develop a vaccine for the new coronavirus.
Vaccines can also pose risks. A small number of people can have dangerous adverse reactions to a vaccine, like severe allergies. In rare cases, vaccines can cause a phenomenon called immune enhancement, where the vaccine makes the recipient’s immune system overreact to the virus target, leading to a more severe disease than in those who were unvaccinated.
Though these risks are small, vaccines have to be delivered to millions of people. That’s why vaccine development focuses so much on safety and reducing the risks of complications as much as possible. Researchers are looking into various ways to speed up development, including human challenge trials where volunteers are deliberately exposed to the virus to test their immunity with and without a vaccine.
Related
What we know right now about Covid-19 immunity and the end of social distancing
Another tactic under investigation is using convalescent plasma. The idea is to harvest the liquid part of blood, including proteins used for clotting, from people who have survived Covid-19. This plasma contains antibodies to the virus, so scientists are seeing whether it can help people with active infections get better. Researchers are also studying whether convalescent plasma can be used as a prophylactic to prevent Covid-19 in the first place.
Companies are also developing antibodies to SARS-CoV-2 using mice genetically engineered to have human immune systems. These antibodies can also be used to treat or prevent the disease.
But antibody transfusions, whether they come from Covid-19 survivors or were created in a lab, only confer protection against the virus for a few months.
Herd immunity, explained
The long-term strategy is to get enough people in a population immune to the virus so that it no longer spreads easily. This is known as herd immunity. It usually requires between 70 and 90 percent of a group of people to be immune in order to be effective, depending on the contagiousness of the virus.
With a large enough share of immunity in the population, even the remaining people who are not immune face a much lower likelihood of being infected. With few susceptible hosts in close proximity, pockets of infection quickly fade out. The question is whether this herd immunity is attained through vaccination or through infection.
The latter would not be ideal since it would involve millions getting sick from Covid-19. The United Kingdom was pursuing this approach back in early March but backed off its herd immunity strategy of limiting restrictions on movement and allowing people to be exposed. The country changed course when forecasters revealed that millions would likely contract the virus, overwhelming the UK’s health system. Sweden has adopted a similar approach and is now facing vastly more Covid-19 cases than its neighbors.
It’s also hard to gauge how close any country is to herd immunity since many people have likely been infected with the virus without knowing it. Figuring this out would require extensive testing for antibodies. And not everyone develops the same level of immunity from an infection. So vaccinating people against Covid-19 is the safer strategy.
Until then, widespread testing to identify the infected, isolating them, and tracing their contacts could help ease some of the pandemic control measures in place now.
How about what we can do as individuals?
Short of drugs like interferons, there isn’t much a person can do to boost their immune system or their response to Covid-19, despite what various supplements promise.
The best Covid-19 approach for individuals is healthy habits — maintain good hygiene, exercise, eat a balanced diet, get plenty of sleep, stay hydrated, manage any chronic health conditions like diabetes, and limit exposure to pollution.
How, in the meantime, do we make decisions without perfect knowledge of Covid-19 immunity?
Though the Covid-19 pandemic has been raging for several months, a lack of key information — from how many people were infected to the origins of the disease — continues to hamper the response.
“More science on almost every aspect of this new virus is needed, but in this pandemic, as with previous ones, decisions with great consequences must be made before definitive data are in,” wrote Harvard epidemiologist Marc Lipsitch in a column in the New York Times.
But the unknowns around immunity to the disease may be the most critical because they stand between the untenable present and a return to normal. Meanwhile, pressure is mounting to relax restrictions on movement to allow life to continue. With incomplete information, policymakers still have to make decisions that depend on immunity, but this can be done in ways that reduce risk.
“The best approach is to construct a conceptual model — a set of assumptions about how immunity might work — based on current knowledge of the immune system and information about related viruses, and then identify how each aspect of that model might be wrong, how one would know and what the implications would be,” Lipsitch wrote.
This is no easy task. It still might be the case that what we learn about immunity may not be enough for everything to go back to normal. We may need to wait, patiently, for a vaccine.
One advantage scientists have in the Covid-19 pandemic that they didn’t have in prior outbreaks is an unparalleled level of information-sharing among researchers around the world. Researchers are posting their preliminary findings online for the world to scrutinize and working across borders, collaborating on an unprecedented scale.
That has led to unknowns becoming known faster than ever. But the disease is continuing to spread, and the drastic pandemic response measures can’t continue forever, so some difficult choices lie ahead.
Support Vox’s explanatory journalism
Every day at Vox, we aim to answer your most important questions and provide you, and our audience around the world, with information that has the power to save lives. Our mission has never been more vital than it is in this moment: to empower you through understanding. Vox’s work is reaching more people than ever, but our distinctive brand of explanatory journalism takes resources — particularly during a pandemic and an economic downturn. Your financial contribution will not constitute a donation, but it will enable our staff to continue to offer free articles, videos, and podcasts at the quality and volume that this moment requires. Please consider making a contribution to Vox today.
Sourse: vox.com





