
Part of
The Vox guide to navigating the coronavirus crisis
Since the beginning of the pandemic, the World Health Organization has stressed that, primarily, Covid-19 spreads through very close personal contact. The virus-laden droplets exhaled from a sick person’s mouth and nose, the thinking goes, are heavy, and fall to the ground before they can get much farther than 6 feet.
But as the pandemic has unfolded, contact tracing studies have shown this isn’t always the case. In China, an air conditioner pushed virus-laden air across three tables in a restaurant, infecting people seated at each one. Researchers reviewed video from the restaurant and saw many of these patrons were more than 6 feet apart from one another, suggesting that the virus traveled through the air.
In Washington state, one person at a choir practice infected 52 of the other participants; it’s thought the singing could have led more virus to linger in the air. Carefully controlled laboratory studies are also suggesting that under the right indoor conditions, SARS-CoV-2, the virus that causes Covid-19, can float in the air and, to a certain degree, spread that way.
Last Thursday, the WHO changed its language to recognize that fact. “Short-range aerosol transmission, particularly in specific indoor locations, such as crowded and inadequately ventilated spaces over a prolonged period of time with infected persons cannot be ruled out,” the WHO now states. Previously, the organization maintained that airborne transmission was unlikely to occur outside the hospital setting, where some procedures can generate super-small particles that linger in the air longer than large respiratory drops.
This change comes after a letter appeared in the journal Clinical Infectious Diseases, co-signed by 239 scientists and engineers, which implored WHO and other public health agencies that “it’s time to address airborne transmission of Covid-19.” With the WHO’s recognition of this mode of transmission, the authors hope, communities can think more about the ventilation of indoor spaces and perhaps engineer solutions to make these spaces safer.
It turns out scientists have been debating whether respiratory diseases like the flu and coronavirus should be labeled “airborne” for a century. More commonly, the “airborne” designation is only applicable to extremely contagious diseases, like measles.
A lot of these terms are confusing (even to the scientists), and they don’t answer the question laypeople care about: Which air is safe to breathe in during the Covid-19 pandemic, and which air is not safe?
To answer that question, it’s helpful to understand two different scientific perspectives on the matter. One is: What physically happens when a sick person breathes, sneezes, or coughs into a room? The other is: What patterns have epidemiologists observed in the way people are exposed to the virus and get sick?
Let’s start with the first.
Big drops versus little drops
There’s a relatively simple, if outdated, way of thinking about how respiratory diseases can spread.
It starts like this: When you exhale, sneeze, or cough, you release a cloud of gas and liquid droplets.
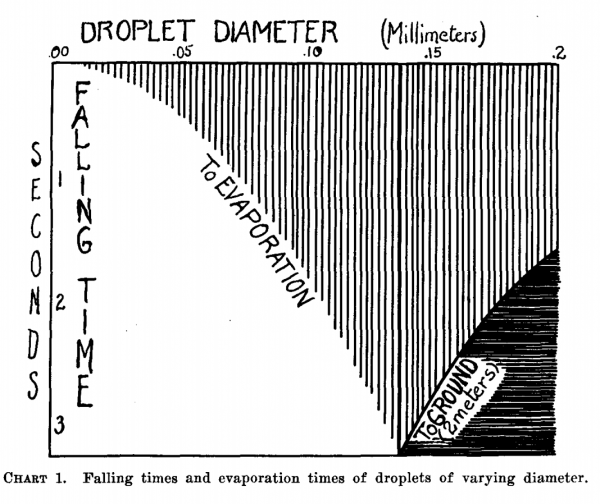
If those droplets are relatively big, they’re heavy and fall to the ground before evaporating, like raindrops do. Others are smaller, and made smaller still by evaporation. These smaller droplets can linger in the air longer, drifting on air currents for perhaps hours. If a droplet is small enough, the moisture in it evaporates before it has the chance to reach the ground (provided the humidity in the room is average). If there’s stuff like germs in that droplet, they become light enough to float on air currents, like the dust you can see suspended in the air. These particles are often called aerosols.
This framework is old, and it comes from William Wells, a scientist who studied tuberculosis transmission in the 1930s. In a 1934 paper, Wells concluded: “It appears, therefore, that transmission of infection through air may take one of two forms depending upon the size of the infected droplet.”
When it comes to Covid-19, one of the first questions epidemiologists tried to answer was: Is the virus spread in the dust that floats or the big drops that fall?
If it’s the small dust, alarm bells go off. These are the prototypical airborne diseases. They include measles, chickenpox, and tuberculosis, and they are extremely contagious. On average, one person infected with measles will infect 12 to 18 others.
If it’s the big drops, it’s still concerning. Diseases like the flu, whooping cough, the common cold, and coronaviruses are primarily large droplet-borne. With these diseases, only the closest contacts to an infected person get infected because large droplets quickly fall to the ground (within 6 feet or so). It’s also possible for these big drops to fall on surfaces, and those surfaces can become contaminated too. Luckily, in the case of Covid-19, there’s a growing consensus that getting sick from touching contaminated surfaces is rare. But keep washing your hands!
(Interestingly, there’s no one reason a new virus, like SARS-CoV-2, would go one route or the other. It’s possible, says University of Leicester virologist Julian Tang, that there may be a difference in the immune response with these airborne diseases that makes saliva and mucous less viscous, leading to more virus in small drops. Also, Tang writes in an email, “it is possible (though no one has studied this yet) that exhaled breath from measles/chickenpox cases may just be shedding much more virus (maybe millions of virus per minute) compared to respiratory viruses, which only exhale 100s to 1000s of viruses per minute.”)
A part of why the terminology here is so confusing, and there’s so much debate about it, is that the words “aerosol” and “droplet” mean different things to different scientific disciplines.
“An aerosol is a particle in the air,” said Lidia Morawska, an engineer and the director of the International Laboratory for Air Quality and Health at Queensland University of Technology. “A droplet is a liquid aerosol.” To her, the distinction between droplets and aerosols doesn’t make any sense. To her, they are all aerosols.
Wells’s droplet versus airborne distinction is still used today. It’s outdated.
Wells outlined a clear distinction between droplets and aerosols according to their size. Big drops fall, and little aerosolized drops float. It’s now appreciated that the actual picture is a lot more complicated.
“We’re always exhaling, in fact, a gas cloud that contains within it a continuum spectrum of droplet sizes,” says Lydia Bourouiba, an MIT researcher who studies the fluid dynamics of infections. And, as she explained in a March paper in JAMA, the conditions of the cloud itself can affect the range of some of the droplets. If propelled by a cough or sneeze, Bourouiba finds, droplets can travel upward of 20 feet. “The cloud mixture, not the drop sizes, determines the initial range of the drops and their fate in indoor environments.”
The speed of the cloud, the temperature and humidity of the environment, and the individual droplet makeup of each cloud determines how long the droplets persist in the air, Bourouiba explained in JAMA.

Which is to say: There are conditions (coughing and sneezing) under which large drops don’t immediately fall to the floor and can spread more than 6 feet away from a person, and they can linger in the air for longer.
There’s growing theoretical evidence for the airborne spread of the coronavirus. Lab studies, in idealized conditions, also show that the virus can live in an aerosolized form for up to 16 hours (the scientists in this case intentionally created aerosolized droplets with a machine).
Another study tracked with lasers the various droplets expelled from a human mouth during speech. It found “normal speech generates airborne droplets that can remain suspended for tens of minutes or longer and are eminently capable of transmitting disease in confined spaces.”
Some studies, the WHO reports, have found evidence of the virus’s RNA in the air of hospital rooms, but notes “no studies have found viable virus in air samples,” meaning the virus was either incapable of infecting others or was in very small quantities unlikely to infect others.
“What we are trying to say is, well, let’s not worry about whether you call it aerosol or whether you call it a droplet,” Morawska, the co-author of the recent commentary imploring the WHO and others to address airborne transmission of Covid-19, says. “It is in the air,” she says, “and you inhale it. It’s coming from our nose from our mouths. It’s lingering in the air and others can inhale it.”
That the WHO updated its language is a sign that it’s starting to appreciate this perspective.
But this perspective is limited. These lab studies can’t perfectly generalize to the real-world conditions in which the virus spreads and infects others. Just because a virus travels far in a drop doesn’t mean it can infect people across great distances. Viruses can degrade quickly outside the body. Also, dose matters. Small exposures to the virus may not be enough to get a person sick.
So to find out how people actually get sick with Covid-19, we need contact tracing studies.
Contact tracing studies show airborne transmission may be possible in confined indoor spaces
Lab studies note the theoretical possibility of airborne transmission. But that’s only one part of the answer to the question “which air is safe to breathe?” Epidemiologists come at this question from another angle, looking at patterns of virus spread observed in the real world and working backward to determine if airborne spread factors in.
Contact tracing studies show us that while droplets being inhaled by people within 6 feet of an infected person explains most of the transmission of Covid-19, there are limited times and environments in which SARS-CoV-2 can behave a bit like an airborne virus.
“So we need to define which types of contact, which type of environments, lead to that type of transmission,” Muge Cevik, a physician and virology expert at the University of St. Andrews, says. In households, she says, an infected person can be isolated in one room and not spread the virus to others in the home (if they remain isolated). A systematic review of studies in The Lancet of both SARS-CoV-2 and similar viruses found large reductions in risk if people just stay 1 meter (3 feet) away from one another. This suggests a lot of the risk of catching Covid-19 is from the large drops that fall quickly to the ground.
But then there are cases where people are packed together in an enclosed space — like a church, with singing or shouting — where the transmission looks a little more like airborne transmission.
The infamous choir practice in Washington state is an example of where airborne transmission might have happened. But what made this event so risky was the convergence of many risk factors: the singing activity (during which the infected person released viral particles into the air), the time spent together (the practice was 2.5 hours), and the interaction between the choir members in an enclosed space (not only did they all practice together, they also split up into smaller groups and shared cookies and tea).
Another study from China investigated an outbreak that started at a Buddhist temple event, tracing much of the spread to the confines of one of the buses transporting people to the function. The bus had one sick person aboard, and 24 out of 67 people on that bus got sick, possibly indicating airborne transmission. Those who sat by the windows fared better, indicating the importance of ventilation.
“I think we just need to get away from this terminology and give much more clear definitions,” Cevik says. For her, it’s about getting people to think critically about which situations are riskier than others. “Risk is a spectrum. It’s not only the distance, but it’s about timing, what type of activities you’re involved in. I know it’s a bit complex, but that’s the reality.”
“Airborne” transmission means something very specific for doctors and health care workers
Perhaps part of the reason the WHO has been slow to address the airborne transmission of Covid-19 is because in a health care setting, “airborne” means a very specific thing.
Though infection prevention experts know there’s a fuzzy boundary between drops that fall and specks that float, the dichotomy between airborne and droplet-borne is baked into how health care workers are trained to respond to outbreaks. “We’ve trained [health care workers] for decades to say, airborne is tuberculosis, measles, chickenpox, droplet is flu and pertussis and meningitis,” Saskia Popescu, a hospital epidemiologist in Arizona, says. “And that’s, unfortunately, kind of antiquated. But that’s how we’ve always done it.”
They do it because there are very specific sets of guidelines in place to deal with extremely contagious airborne diseases in a hospital setting. For instance, a patient with a dangerous airborne disease often needs to be put in a room with an air pressure lower than the rest of the rooms in the building. That way, no virus in the air of that room can escape it (since air flows from high pressure to low pressure).
For droplet transmission, health care workers can be a little more lax; they can wear simple surgical masks during routine care and can save high-filtration (and sometimes scarce) respirators for the most dangerous procedures and cases.
In this light, it makes some sense that the WHO has been hesitant to label Covid-19 an “airborne” infection. It’s not an airborne infection like measles is. It is not as contagious. Contact tracing studies consistently find that Covid-19 is spread most readily among people in the closest physical contact to one another. “Airborne” means something very specific, very resource-intensive, and very scary for hospitals and the people who work in them. And Covid-19 doesn’t match that definition.
“The debate often isn’t very nuanced because of these rigid categories,” Daniel Diekema, an infectious diseases physician and epidemiologist at the University of Iowa, says. “As soon as you say ‘airborne’ in the hospital infection prevention world, it brings to mind pathogens like tuberculosis, measles, chickenpox. It’s clear the respiratory viruses, influenza, coronaviruses, are not airborne in the same way that the measles, varicella [chickenpox] become airborne.”
But at the same time, with Covid-19 and other respiratory viruses, “there definitely are small-particle aerosols produced,” he says. “And in the right setting, where there’s poor ventilation, indoors, and a crowded environment, there is a risk for transmission among individuals, even if they may be more than 6 feet apart.”
So what do we do with this information?
Neither contact tracing studies nor lab studies can perfectly answer the question of “which air is safe?” But that’s science for you. Scientists use imperfect methods, attacking from many angles, to try to arrive at the truth, which can take a while to nail down precisely.
Overall, the recognition that Covid-19 can spread through the air shouldn’t really change how we, individually, protect ourselves and others against it. Six feet of distance between people is still a good barrier to prevent spread via large drops. Mask-wearing could help prevent both large drops and small drops from being released in the first place. Time matters too: the longer we spend in an enclosed, poorly ventilated space with others, the greater the chances of being exposed to an infectious dose of the virus.
The bottom line, as a trio of engineers from Clarkson University writes in the Conversation, is that “while staying six feet from other people reduces exposure, it might not be sufficient in all situations, such as in enclosed, poorly ventilated rooms.”
We still need to think about the environments we’re in: Indoors is much riskier than outdoors (where greater airflow can disperse drops and aerosols more quickly, and where the environment is less conducive to SARS-CoV-2 survival). And indoors, ventilation can make a big difference. An indoor space where the air is constantly refreshed with air from the outdoors is better than one where the air is stagnant.
We also still need to think about the activity we’re engaging in. Shouting, singing, and other such activities produce more droplets (of any size) than just sitting quietly.
Morawska hopes that in bringing attention to airborne spread of Covid-19, there can be more attention paid to engineering solutions for indoor spaces to mitigate the spread of the pandemic.
Public health officials have continually stressed social distancing, mask-wearing, and hand-washing as ways to stop the spread of Covid-19. “But have you ever heard a restaurant reopening announce they’ve improved ventilation or increased ventilation? No. This is really the point,” Morawska says. If Covid-19 is in indoor air, we should also be doing something about the air.
Support Vox’s explanatory journalism
Every day at Vox, we aim to answer your most important questions and provide you, and our audience around the world, with information that has the power to save lives. Our mission has never been more vital than it is in this moment: to empower you through understanding. Vox’s work is reaching more people than ever, but our distinctive brand of explanatory journalism takes resources — particularly during a pandemic and an economic downturn. Your financial contribution will not constitute a donation, but it will enable our staff to continue to offer free articles, videos, and podcasts at the quality and volume that this moment requires. Please consider making a contribution to Vox today.
Sourse: vox.com






