
At the age of 89, my grandfather walked into the family room from his bedroom, forgetting he needed his walker. We’re still not quite sure exactly how he stumbled and hit the ground, but he ended up with a hip fracture.
His doctors deemed him too high-risk for surgery, and so he was left bedbound for the next year until his immobility, along with another health issue, became too debilitating and he died.
Since his death, my family has often discussed how that one fall — and his undiagnosed osteoporosis that was revealed with the hip fracture — was the beginning of the end for him.
We also can’t get over how less than a year later, in the very same room where my grandfather fell, my grandmother stumbled and fractured her left arm in three places. Previously fully independent, she then required 24/7 care because she couldn’t even use the bathroom without assistance.
As a physician, what has disturbed me most is that both my grandmother and grandfather had the same primary care doctor, who never bothered to do bone density scans to see if they had osteoporosis.
And it’s precisely the health care system’s failure to look for osteoporosis as often as it should — along with a parallel crisis in osteoporosis treatment — that is setting us up for the acceleration of a disturbing trend that was recently highlighted in an important study.
Researchers writing in the journal Osteoporosis International found that hip fractures in women over 65 began increasing in 2013 among Medicare recipients (after plateauing for years), with an additional 11,000 estimated hip fractures between 2013 and 2015. There are two clues that point at the causes of this burgeoning crisis: There’s been a decrease in bone density screening tests and a decrease in prescriptions for osteoporosis medications (the biggest class of which are called bisphosphonates) because of patients’ fears of their side effects.
So if doctors aren’t looking for osteoporosis, and many patients are turning down treatment, how can we prevent life-altering falls like those suffered by my grandparents?
More than 10 million Americans have osteoporosis today
More than 10 million Americans currently have osteoporosis, and another 44 million are at increased risk of developing it. By 2020, the number of Americans with low bone density is expected to rise to 64 million adults, or 20 percent of the population, with a proportional increase in the number of fractures.

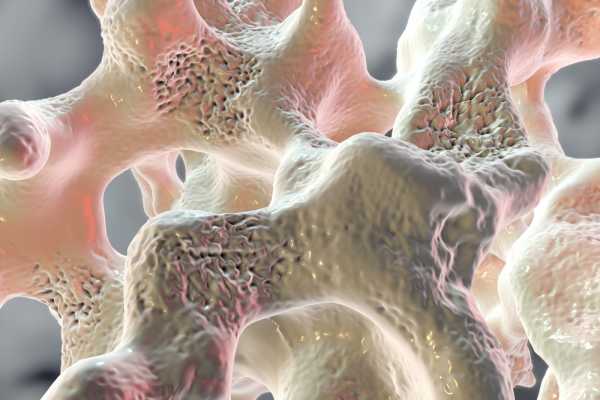
In osteoporosis, which means porous bone, bone density is decreased because of not enough bone formation, excess bone loss, or some combination of both.
Most commonly, this loss of bone density occurs due to hormonal changes that accompany aging: lower estrogen levels in women post-menopause and decreasing testosterone levels in men over the age of 70.
Other factors — such as the use of certain medications, autoimmune disease, tobacco use, excess alcohol intake, and low calcium levels — can amplify bone loss or dampen bone building, thus increasing the risk for osteoporosis.
The lifetime risk of an osteoporotic fracture (fractures that occur at a site with known low bone density) is estimated to be 40 to 50 percent in women and 13 to 22 percent in men. We have long known that more than 30 percent of people will die within one year after suffering a hip fracture, like my grandfather did. This same study from the early 1990s noted increasing mortality for those suffering fractures at older ages, with those over the age of 90 facing 66 percent mortality in the year following proximal femur fractures.
And if you survive the first year, increased mortality following osteoporotic hip fractures extends 10 years past the fracture itself. Even for those who survive their hip fracture, most will be unable to regain their full prefracture function and mobility.
The heightened risk of death aside, the additional health care costs following hip and vertebral fractures are staggering. In the first year following hip fracture, the incremental cost was estimated to be $10,000, according to a study published in the late 1990s.
Similarly, a study used a sample from the population of 30.2 million Medicare recipients in 2002 finding that on average, fractures created an annual medical cost of $8,600 for the 1.6 million Medicare recipients who suffered fractures that year. The quick math on this then places a cost of nearly $15 billion for the American health care system from fractures alone. And for women over the age of 55, hospitalizations and their associated costs for osteoporotic fractures are greater than for heart attacks, strokes, or breast cancer.
The diagnosis of osteoporosis is determined either by bone density screening or when a patient incurs what is known as a fragility fracture. So many of my osteoporosis patients have told me that they are careful and will make sure they do not have a fracture in an attempt to avoid additional medications.
But sadly, osteoporosis doesn’t quite work like that. When a minor fall culminates in a fracture, it is deemed a fragility fracture and can result in an osteoporosis diagnosis in and of itself. Our family was as careful as we could be with my grandfather, but one little misstep still led to a hip fracture.
How Medicare cuts drove down osteoporosis screening
If we’re not screening for osteoporosis, then we’re not going to find it. So why exactly aren’t more doctors doing screenings?
Currently, the US Preventive Services Task Force (USPSTF) recommends osteoporosis screening in women age 65 and older and in younger women who may have equivalent or greater fracture risk due to other risk factors. The USPSTF does not provide a screening recommendation for men, which is problematic in and of itself, but there are other authorities that recommend screening men for low bone density at the age of 70.
One component of decreased screening may simply be physician oversight of current guidelines. But the bigger culprit is likely the 2007 Medicare reimbursement cuts for osteoporosis screening.
The way doctors estimate bone strength is by measuring bone mineral density. The most common way to do it is with a dual-energy X-ray absorptiometry (DXA or DEXA) scans, which are noninvasive tests with minimal cost and negligible radiation risk.
It’s estimated that the 2007 Medicare reimbursement cuts ultimately led to 800,000 fewer DXA scans than expected, screening tests that might have prevented 12,000 fractures. The decline in reimbursements has made DXA screening cost-prohibitive for many physician practices, thereby making DXA tests less widely available to patients as well.
Osteoporosis treatment is not as scary as it seems
With fractures on the rise, focusing on the management of osteoporosis is now even more important. Calcium and vitamin D can improve bone mineral density, but these alone do not reduce fracture risk. So other therapies should be offered to patients with osteoporosis, including exercise with weights, fall prevention guidance, and medication.
The class of antiresorptive medications known as bisphosphonates have been used since the 1990s and remain one of the most widely used osteoporosis medications. Available as oral medications or intravenous infusions, both forms of bisphosphonates have been shown to reduce fracture risk, prevent recurrent hip fractures, and reduce the risk of death after hip fractures.
Unfortunately, bisphosphonates also have the possibility of the very rare side effects of atypical fractures and jaw osteonecrosis. And a spike in media reports of spontaneous bone breakage and crumbling jaws coincided with the 50 percent drop in bisphosphonate use from 2008 to 2012.
Three large placebo-controlled, randomized studies that included more than 15,000 patients found only 12 fractures could be related to bisphosphonate use — that’s less than a tenth of a percent of patients studied. Additionally, a task force commissioned to look specifically at the risk for jaw osteonecrosis associated with bisphosphonates used for osteoporosis treatment found that it is very low, estimated to be between one in 10,000 and less than one in 100,000 patient years.
Fears of these side effects have led many clinical guidelines to call for bisphosphonate “holidays” to try to further minimize the risk of these rare complications on patients who have been on bisphosphonates for three to five years. But Dr. Kenneth Saag, a professor of medicine at the University of Alabama Birmingham and the current president of the National Osteoporosis Foundation, argues that these drug holidays may actually do more harm than good for many patients. Saag and other physicians who have been using these medications for years in high-risk patients understand that the benefits from bisphosphonates in preventing typical fractures outweigh the risks of any of these unusual complications.
If my grandparents had been given the opportunity to gamble on a one-in-1,000 chance of an unusual side effect versus a one-in-two chance of suffering an osteoporotic fracture, then I’m sure they would have opted for bisphosphonate treatment. They just never got the chance to place their bets before the odds stacked against them.
Do we stand a chance against this osteoporosis crisis?
It’s no small wonder that a drop in osteoporosis screening and a decrease in the utilization of osteoporosis medications has caused hip fracture rates to rise. The biggest issue is that without screening, there is virtually no way to diagnose osteoporosis until a fracture occurs.
Perhaps if reimbursements for DXA scans improved, then more practices would be able to afford the machines to provide this test for their patients. But with even more Medicare cuts looming, this may not be our best bet. Maybe the least we can do is “capture the fracture” and treat osteoporosis after the identifying injury.
Fracture liaison services (FLS) are designed to do just this. FLS teams try to reduce future fracture risk in patients who present to hospitals following fractures. Typically, the FLS team is led by a physician who is a bone health expert and team of other providers who help channel patients into appropriate osteoporosis care. The goal is for the FLS team to identify patients who need osteoporosis treatment as close as possible to the time they suffer their initial bone injury.
With 80 percent of fracture patients never even being offered osteoporosis screening or treatment, there is an undeniable need for the expansion of FLS programs to provide the best care for fracture patients. These services will be critical to preventing secondary fractures, and, according to Saag, osteoporosis treatment “can reduce the rates of recurring vertebral and hip fractures by up to 70 percent and 50 percent, respectively.”
My grandfather never had the luxury of an FLS team. But when my grandmother suffered a major osteoporotic fracture, I essentially functioned as her personal FLS. She left the emergency room with her arm in a sling with a follow-up appointment to see an orthopedic doctor, while her primary care doctor prescribed home physical therapy and nothing else. The only reason my grandmother saw an osteoporosis specialist for treatment after her fall was because I intervened and insisted that a referral be placed.
But the bigger problem is this: The American health care system is blasé about bone health, especially in the elderly, and that needs to change before this crisis spirals out of our control.
Farah Naz Khan is a doctor and a writer in Seattle. Find her on Twitter @farah287 or via FarahNazKhan.com.
Sourse: vox.com






