It’s one of the mysteries that has puzzled cancer epidemiologists: Why are younger and younger people becoming sick with colorectal cancer?
In 2017, researchers at the American Cancer Society showed colorectal cancer is rising sharply in younger generations. For people in their 20s and 30s, colon cancer rates increased 1 to 2 percent between the mid-1990s to 2013. And rectal cancer rate shot up even more dramatically — rising 3 percent per year in the same age cohort.
Overall, those born in 1990 have double the risk of developing colon cancer and four times the risk of getting rectal cancer compared to those born around 1950. So in response to the alarming trend, in 2018 the society lowered the age for routine colorectal cancer screening to 45 from 50.
“It’s not like the problem is bad and has stabilized,” said Thomas Weber, the director of surgical oncology at New York’s Northwell Health, who organizes an annual summit for researchers trying to solve the mystery. “The problem has continued to worsen.”
But a new study published Thursday in JAMA offers one potential explanation: the rising rates of obesity.
Since 1980, the obesity prevalence has doubled in more than 70 countries around the world. Thirty-nine percent of US adults, are now obese, along with 19 percent of children and adolescents.
The JAMA study looked at 85,000 women and found a link between a higher body weight, particularly obesity, and a greater risk of colorectal cancer.
But not so fast: One of the study’s authors, Harvard cancer epidemiologist Yin Cao, warned this study isn’t the final answer: “I think we are getting closer but this is not the final answer for [the mystery].” Here’s why.
The link between obesity and colorectal cancer
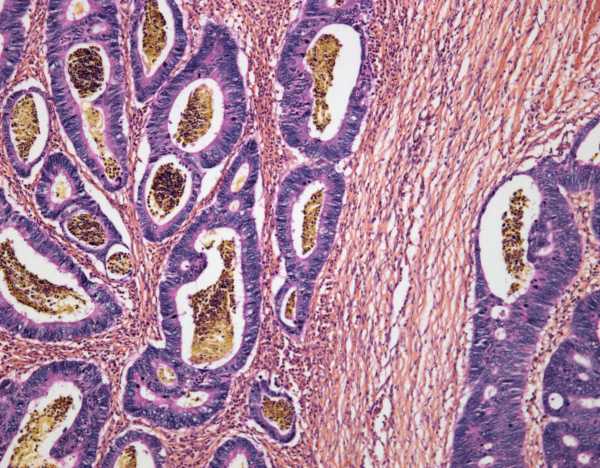
Colorectal cancer is the third most common cancer diagnosed in the United States, with a lifetime risk of 4 to 5 percent in men and women. While it used to be a disease that mainly surfaced after middle age, the shift to younger and younger ages has alarmed researchers. And not only are people in their 20s and 30s increasingly being diagnosed with the disease; they’re also dying from it.
The main reason obesity is thought of as a potential driver of early-onset colorectal cancer is because its associated with inflammation in the body.
You can think about inflammation in two ways. There’s helpful inflammation, as with your body’s immune response to an attack by a foreign invader — your skin reddens and heats up to fight off bacteria in a cut.
There’s also harmful, or chronic, inflammation: when your body’s inflammatory response goes into overdrive, hampering its ability to fight off viruses and disease. One measure of it is a blood marker called C-reactive protein (CRP). Researchers have found associations between higher levels of CRP and various chronic illnesses, including cancer, arthritis, cardiovascular disease, and diabetes. People who are inactive or obese or who eat an unhealthy diet seem to have higher levels of CRP in their systems too.
The new JAMA study looked at 85,000 women aged 25 to 42 who were followed from 1989 to 2011 as part of the ongoing Nurses’ Health Study II. The researchers mapped early-onset colorectal cancers against body mass index (BMI) — both current and at age 18 — to figure out whether having a higher BMI at any point in a person’s life was associated with greatest colorectal cancer risk before age 50. And they found strong associations.
The 114 women who developed colorectal cancer in the study tended to have a higher BMIs. Their risk also increased the higher their body weights climbed. So people with obesity (a BMI of 30) had nearly double the risk of early-onset colorectal cancer compared with women in the normal BMI range (18.5 to 22.9). In other words, it looked like as obesity rates climb, so too does colorectal cancer risk.
Why this mystery is hard to solve
But the impact of obesity on cancer risk is pretty hard to untangle from other behaviors or attributes people with obesity may have, like diet. Scientists have found strong associations between Western-style, pro-inflammatory diets — heavy in processed meat, red meat, organ meat, sugary beverages, and refined grains — and a higher risk of colorectal cancer. And it’s possible the heavier people in the new study followed a diet that was more inflammation-promoting.
What’s more, the number of patients with early-onset colorectal cancer was also very small relative to all the people who get the disease. “There were 114 cases under the age of 50, and there are some 16,000 cases a year of colorectal cancer of people under the age of 50 in the US,” Weber said. So the study only looked at a subset of cases.
So while obesity may play a role in driving this alarming trend, it’s probably not the entire explanation. Weber added: “Many, many providers are struck by how fit and active many of their young colorectal cancer patients are. And this includes the fact the vast majority of these cases have nothing to do with hereditary syndromes.”
Sourse: vox.com






