
Medicaid expansion is a rich tapestry. States, those laboratories of democracy, have implemented varying programs to expand Medicaid under the Affordable Care Act. Some have cleanly expanded, others have instituted cost-sharing requirements or moved beneficiaires to private insurance, and now, under the Trump administration, some states are starting to require Medicaid enrollees to work or else lose coverage. Of course, we also still have 17 states that have refused to expand Medicaid at all.
This provides us a unique opportunity to assess the consequences of these different policies, and new research published in Health Affairs this week is maybe the most detailed portrait yet of what happens under these various approaches.
The Harvard researchers, led by Benjamin Sommers, surveyed people who would be eligible for Medicaid expansion in three states: Ohio, Indiana, and Kansas.
vox-mark
VoxCare
Subscribe
By signing up, you agree to our Privacy Policy and European users agree to the data transfer policy.
For more newsletters, check out our newsletters page.
- Ohio expanded Medicaid in 2014, using its traditional Medicaid program.
- Indiana expanded Medicaid in 2015, using a federal waiver. It required beneficiaries to make a monthly contribution to a health savings account or they could lose certain benefits. Some enrollees could even be locked out of coverage entirely if they failed to make those payments.
- Kansas has not yet expanded Medicaid.
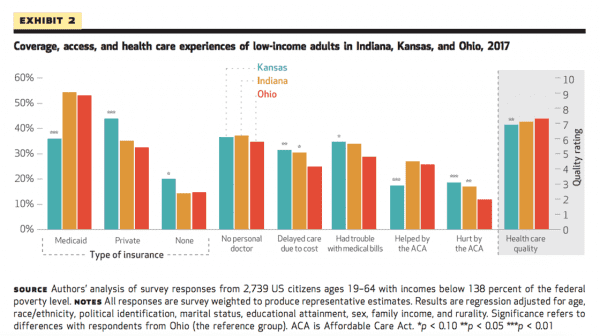
This chart summarizes their findings nicely.
(The survey reached more than 2,700 Medicaid expansion-eligible people across the three states. For state-specific or situation-specific questions, the sample is obviously smaller.)
Unsurprisingly, Ohio and Indiana had higher levels of Medicaid coverage and lower uninsured rates for the expansion population than Kansas did.
The most striking findings were in health care access: In Indiana, with its cost-sharing requirements and lock-out provision, the Medicaid expansion population was substantially more likely to delay care because of its cost or to have trouble paying their medical bills compared to the same population in Ohio, which did not ask expansion enrollees to pay much out of pocket.
The unavoidable suggestion is, as the researchers wrote, that “Indiana’s waiver program led to less affordable care than Ohio’s traditional expansion of Medicaid did.”
The Harvard researchers asked a few more detailed of their Indiana respondents. They found that four in 10 Medicaid expansion eligible people had never heard of the health saving accounts they were supposed to pay money into in order to receive full coverage (including vision and dental and more generous prescription drug benefits), and 25 percent said they knew about those accounts but still didn’t contribute money.
Among the people who knew about the Medicaid health savings accounts but who weren’t making payments:
- 30 percent said they couldn’t afford it.
- 22 percent said they did not think the payments were worth it.
- 19 percent said that they were confused about the accounts.
Among the uninsured in Indiana who were not enrolled in the Medicaid expansion program:
- 30 percent said it was unaffordable.
- 20 percent said they thought they didn’t qualify.
- 17 percent said it was too complicated.
“Taking into account the substantial confusion about Indiana’s program and its cost-sharing requirements, it is perhaps not surprising that difficulties affording care were higher in Indiana than in Ohio, which implemented a traditional Medicaid expansion with minimal cost sharing,” the authors wrote.
One other note, from Kansas, which is considering instituting a work requirement: Forty-nine percent of Medicaid expansion-eligible people said they were already working and 34 percent said they were disabled. That tracks with data we’ve seen elsewhere suggesting that most people who might be the subject of a Medicaid work requirement either are working or would not be expected to work. Just 11 percent said they weren’t working now, but a work requirement would motivate them to look for work.
Here was the big-picture takeaway from the Harvard researchers:
This goes back to the foundational debate about Medicaid: Is the program meant to ensure vulnerable people have access to health care or is it meant to do something else, like encourage people to work and improve their economic station?
Because if it’s the former, as many advocates believe, then these findings indicate the policies being pursued by Indiana and other states, supported by top officials in the Trump administration, are failing in that mission.
This story appears in VoxCare, a newsletter from Vox on the latest twists and turns in America’s health care debate. Sign up to get VoxCare in your inbox along with more health care stats and news.
Join the conversation
Are you interested in more discussions around health care policy? Join our Facebook community for conversation and updates.
Sourse: vox.com






